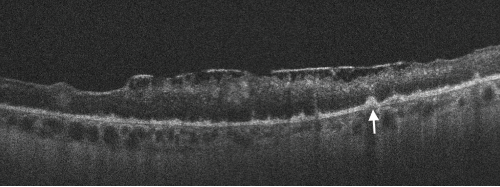
Figure 2. Spectral domain optical coherence tomography (SD-OCT) of the left eye with hyper-reflective retinal pigment epithelial (RPE) nodularity (white arrow) and overlying loss of normal photo receptor architecture.
Discussion
Ocular syphilis is rare and tends to occur at any stage of the disease. However, it is commonly associated with neurosyphilis. Its incidence has been increasing in the developed countries for the past few years. This may be related in part to decreased condom use in high-risk populations following the advent of highly active anti-retroviral therapy (HAART).5
Because its clinical manifestations vary, ocular syphilis is a big masquerader and may be challenging to diagnose. Ocular symptoms are commonly non-specific and may lead to a delay in diagnosis and treatment. New-onset, monocular, blurry vision is usually an early manifestation; however, other non-specific systemic symptoms can mask the diagnosis.
The clinical presentation of monocular vision changes when present with relevant associated symptoms can be concerning for GCA, which can lead to permanent visual loss if untreated. Therefore establishing a definitive diagnosis is paramount.
Elevated inflammatory markers may be present in both conditions. Patients with such a presentation are often empirically treated with high-dose systemic steroids and can be subjected to a temporal artery biopsy. Because the diagnostic yield of a temporal artery biopsy is low, these patients can remain on treatment despite a negative biopsy result. A diagnosis of ocular syphilis in such cases can be missed, resulting in permanent visual impairment. A timely diagnosis of this important clinical entity can mitigate unnecessary testing and prevent complications.
Based on our experience, we recommend testing for syphilis and tuberculosis prior to initiating systemic steroid therapy. Additionally, a detailed sexual history must be obtained, and those with high-risk behaviors must also be tested for syphilis.
Iryna Nemesh, MD, is a rheumatology fellow in the Department of Medicine, Division of Rheumatology, Medical College of Wisconsin Affiliated Hospitals, Milwaukee.
Saleema Kherani, MD, MPH, is an ophthalmology resident in the Department of Ophthalmology, Medical College of Wisconsin Affiliated Hospitals, Milwaukee.
Shikha Singla, MD, is an assistant professor in the Department of Medicine, Division of Rheumatology, Medical College of Wisconsin Affiliated Hospitals, Milwaukee.
William Wirostko, MD, is a professor of vitreoretinal surgery and ocular oncology in the Department of Ophthalmology, Medical College of Wisconsin Affiliated Hospitals, Milwaukee.
References
- Doris JP, Saha K, Jones NP, Sukthankar A. Ocular syphilis: The new epidemic. Eye (Lond). 2006 Jun;20(6):703–705.
- Majumder PD, Chen EJ, Shah J, et al. Ocular syphilis: An update. Ocul Immunol Inflamm. 2019;27(1):117–125.
- Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005;20(3):161–167.
- Biousse V, Newman NJ. Ischemic optic neuropathies. N Engl J Med. 2015 Jun 18;372(25):2428–2436.
- Fonollosa A, Giralt J, Pelegrín L, et al. Ocular syphilis-back again: Understanding recent increases in the incidence of ocular syphilitic disease. Ocul Immunol Inflamm. 2009 May–Jun; 17(3):207–212.


