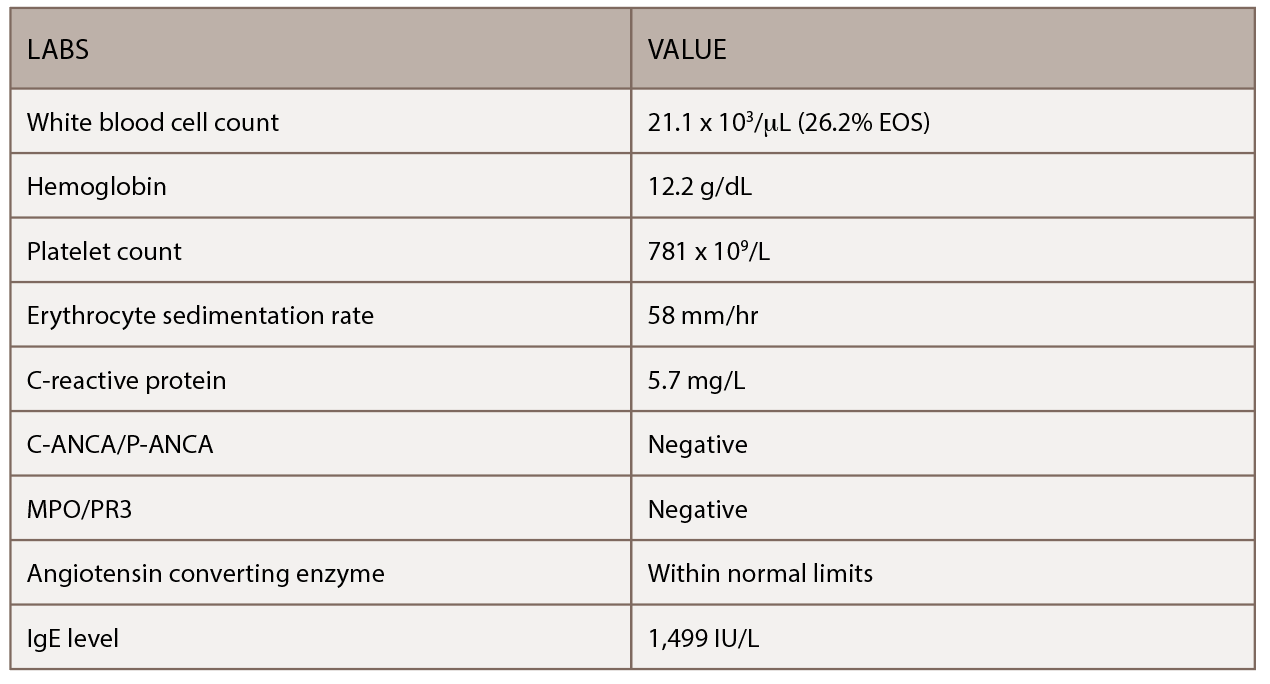
(click for larger image) Table 1: This table shows the patient’s initial outpatient rheumatology serologic workup.
In our emergency department, the patient was immediately evaluated for worsening shortness of breath and wheezing, which were unresponsive to albuterol. He did not have a fever and denied any weight loss, night sweats, headaches, visual changes, rash or joint pain. The patient had diarrhea and distal lower extremity weakness with numbness and tingling of his feet (more so on the left than the right). His vital signs were stable, and labs revealed mild anemia, leukocytosis of 32,000/µL (upper limit of normal [ULN]: 11,000/µL), 39.4% eosinophils (ULN: 3%), thrombocytosis at 791,000/µL (ULN: 450,000/µL) and an elevated paraprotein gap (total protein-albumin >4).
An electrocardiogram (ECG) proved unremarkable. Serial cardiac enzymes demonstrated evidence of myocardial injury (first set: troponin 0.95 units, which increased to 2.1 units ng/mL). The ECG demonstrated a normal ejection fraction without diastolic dysfunction in the setting of a pericardial effusion and a mildly dilated inferior vena cava. Cardiac catheterization did not show any evidence of obstructive coronary artery disease. The patient was clinically diagnosed with myocarditis and was given aspirin, atorvastatin and metoprolol.
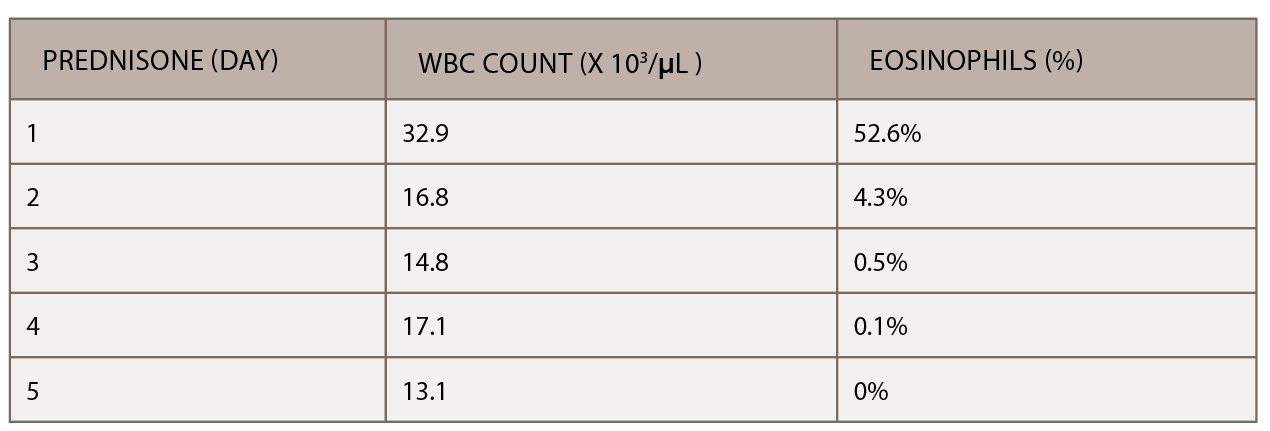
(click for larger image) Table 2: The initiation of inpatient prednisone produced a down-trending white blood cell count and normalization of percentage of eosinophils.
A chest CT demonstrated a persistent parenchymal opacity in the right upper lobe, with improved left upper lobe aeration compared with the prior left upper lobe opacity (see Figure 2). A sinus CT demonstrated severe sinonasal mucosal disease with near complete opacification of the bilateral frontal and ethmoid sinuses (see Figures 3 and 4). Inpatient labs revealed elevated inflammatory markers and a markedly elevated rheumatoid factor (RF) of greater than 600 IU/mL. With concern for underlying systemic vasculitis, we initiated prednisone at 1 mg/kg/day, and subsequent labs demonstrated a drop in white blood cells and normalization of his eosinophil percentage (see Table 2). The patient noted subjective improvement in his wheezing, diarrhea and motor strength.
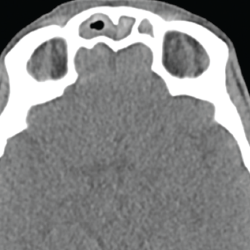
Figure 3. This sinus CT shows severe nasomucosal disease with near complete opacification of the bilateral frontal sinuses.

Figure 4. This sinus CT shows severe nasomucosal disease with near complete opacification of the bilateral ethmoid sinuses.
An esophagogastroduodenoscopy (EGD) and colonoscopy demonstrated chronic gastritis and patchy areas of severely congested, erythematous and friable mucosa throughout the entire colon. A bronchoscopy with bronchoalveolar lavage and a transbronchial lung biopsy showed bronchiole walls with a reticular basement membrane containing scattered infiltrates of eosinophils in the adventitia (see Figure 5). Fine needle aspiration of lymph nodes ruled out epithelial malignancy. Before the EGD and colonoscopy, active gastrointestinal bleeding was ruled out, and the decision was made to administer a reduced pulse dose of intravenous methylprednisolone at 500 mg/day for three days to hasten neurologic recovery.
Prior to discharge, the patient underwent a left sural nerve biopsy, which showed vasculitic neuropathy with endoneurial fibrosis. Pathology demonstrated arteries in longitudinal sections with thrombosis and eosinophils mixed with macrophages and T cells, consistent with vasculitis (see Figure 6). The patient experienced mild improvement of his neuropathy and was subsequently discharged on prednisone 1 mg/kg/day with outpatient rheumatology follow-up.



