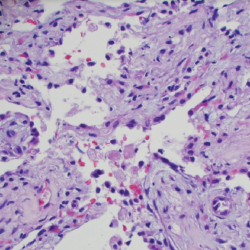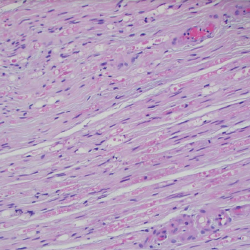
Figure 6. A sural nerve biopsy demonstrated arteries in longitudinal sections with thrombosis and eosinophilic infiltrate, consistent with vasculitis.
Discussion
EGPA was first described more than 60 years ago, but its underlying mechanisms remain poorly understood. The 1990 ACR classification criteria for EGPA include: 1) asthma, 2) eosinophilia (>10% of total white cell count), 3) neuropathy, 4) non-fixed pulmonary infiltrates, 5) paranasal sinus abnormality and 6) extravascular eosinophil infiltration on biopsy.6 For classification purposes, a patient is said to have EGPA if at least four of these six criteria are present (sensitivity of 85%; specificity of 99.7%).6
Outside the ACR criteria, additional classification criteria exist for EGPA. Per the 1984 Lanham classification criteria, a patient has a diagnosis of EGPA if all three of the following criteria are present: 1) asthma, 2) eosinophilia (>10% WBC count or >1.5×109) and 3) systemic vasculitis affecting at least two extrapulmonary sites.7