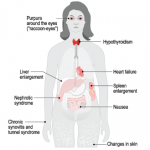
Amyloidosis is a condition consisting of several distinct clinical entities sharing the common pathological feature of protein misfolding, resulting in fibrils consisting of a highly structured, stable, beta-sheet confirmation prone to binding with other like molecules.
Within the scope of rheumatology, three distinct conditions come to mind when considering neck masses, per a study performed by Knopf et al.: 1) Sjögren’s syndrome, where neck involvement is typical; 2) granulomatous with polyangiitis, in which upper airway and sinonasal manifestations often precede systemic manifestations; and 3) sarcoidosis, in which pulmonary manifestations dominate, although isolated head and neck presentations may appear.3
In the study, head and neck symptoms suggestive of Sjögren’s included sicca and salivary gland enlargement, followed by lymphadenopathy and facial swelling.3 Patients diagnosed with granulomatosis with polyangiitis experienced a broad spectrum of head and neck symptoms, the majority being sinonasal tract and middle ear related, including rhinorrhea, facial and cranial pain, otorrhea, dyspnea and dysphonia, recurrent epistaxis and diploplia.3 Sarcoidosis head and neck symptoms included lymphadenopathy, salivary gland enlargement, sicca, facial and cranial pain, rhinorrhea and facial palsy.
Of course, both infectious and neoplastic conditions remain high on the differential with any of the above presenting symptomatology.3
The time course of presentation (i.e., acute, subacute, chronic) of a neck mass may hold substantial bearing on determining etiology. Typically, neck masses seen in an acute presentation tend to be symptomatic, with the most common causes of cervical lymphadenopathy being attributable to infection or inflammation created by a wide variety of odontogenic, salivary, viral and bacterial etiologies.4 These lymph nodes are often tender, swollen and mobile, and can be erythematous and warm to the touch.
In our case, although the presentation was described as acute (appearing over the span of one to two days), it was an unusual time course for the given etiology of amyloidosis, which has more typically been encountered as a subacute presentation over a period of several weeks to months. Subacute masses are classified as occurring within weeks to months, and although they may grow fairly quickly, they often go unnoticed at onset due to their asymptomatic nature.4
Persistent asymptomatic neck masses in an adult should, in general, be considered malignant until proven otherwise.4 This certainly was of prime concern for us, regardless of the duration of our patient’s neck mass. Note: Biopsy is appropriate if an abnormal lymph node has not resolved after four to six weeks, and it should be performed promptly in patients with other findings suggestive of malignancy, such as night sweats, fever, weight loss or a rapidly growing mass.4
In subacute neck masses, amyloidosis falls under less commonly encountered etiologies, alongside lymphoma, metastatic cancers, parotid tumors, sarcoidosis and Sjögren’s, while the most common causes include metastatic squamous cell carcinomas of the aerodigestive tract.4 Rarely encountered subacute masses are most often the result of Castleman disease, Kikuchi disease, Kimura disease and Rosai-Dorfman disease.4
The initial diagnostic test of choice in an adult with a persistent neck mass is contrast-enhanced CT, which provides valuable initial information regarding the size, extent, location and content or consistency of the mass.5 Additionally, contrast media may help identify malignant lymph nodes that are not enlarged, and distinguish vessels from lymph nodes.5 Avoid iodine-based contrast media in patients with a history of thyroid disease or when metastatic thyroid cancer is a concern.5
Although PET-CT can be used to distinguish between malignant and unaffected tissues, its use in preliminary diagnosis is not as effective and should be limited to managing a malignancy.5 Ultrasonography may also help guide fine needle aspiration of non-palpable or small superficial lesions.5 Although CT and ultrasonography share similar capabilities, ultrasonography is preferred initially in young patient populations to reduce radiation exposure. It may also be preferred to avoid contrast media-induced nephropathy in patients with underlying renal disease.
CT angiography is recommended for evaluating a pulsatile neck mass and is preferred over magnetic resonance angiography.5 The clinician may proceed with fine needle aspiration (if indicated) once appropriate imaging has ruled out involvement of underlying vital structures.5 Fine needle aspiration can provide further information through cytology, flow cytometry, Gram stain, and bacterial and acid-fast bacilli cultures while avoiding complications of open biopsy.4