Summary
We described a case of biopsy-proved RCEV that presented with punched, ulcerative skin lesions and no peripheral eosinophilia, both of which are unusual features rarely reported in the literature. RCEV is uncommon, but should remain on the differential diagnosis of necrotizing vasculitis with or without eosinophilia. Although prednisone was effective, the skin lesions recurred with prednisone taper, resulting in prolonged steroid use and multiple side effects.
Limited data exist to guide RCEV treatment, with only one case report of a patient successfully treated with tacrolimus, two with dapsone, one with indomethacin and one with suplatast tosilate.5,7,8,15 Our patient did respond to azathioprine, suggesting its potential use in RCEV. Whether other immunosuppressive agents, such as mycophenolate or cyclophosphamide, would provide any benefit in severe cases remains unclear.
 Julia Tan, MD, is an internal medicine resident at the University of British Columbia, Vancouver, Canada.
Julia Tan, MD, is an internal medicine resident at the University of British Columbia, Vancouver, Canada.
 Kun Huang, MD, PhD, is a rheumatologist at the University of British Columbia, Vancouver, Canada.
Kun Huang, MD, PhD, is a rheumatologist at the University of British Columbia, Vancouver, Canada.
 Natasha Dehghan, MD, is a rheumatologist at the University of British Columbia, Vancouver, Canada.
Natasha Dehghan, MD, is a rheumatologist at the University of British Columbia, Vancouver, Canada.
 Neda Amiri, MD, is a rheumatologist at the University of British Columbia, Vancouver, Canada.
Neda Amiri, MD, is a rheumatologist at the University of British Columbia, Vancouver, Canada.
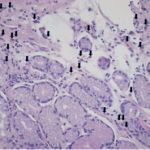
Acknowledgment: The authors thank Martin Trotter, MD, PhD, head of the Department of Pathology and Laboratory Medicine at Providence Health Care, University of British Columbia, Vancouver, Canada, for reviewing and preparing the histopathology images of this manuscript.
References
- Chen KR, Pittelkow MR, Su D, et al. Recurrent cutaneous necrotizing eosinophilic vasculitis. A novel eosinophil-mediated syndrome. Arch Dermatol. 1994;130(9):1159–1166.
- Launay D, Delaporte E, Gillot JM, et al. An unusual cause of vascular purpura: Recurrent cutaneous eosinophilic necrotizing vasculitis. Acta Derm Venereol. 2000 Sep–Oct;80(5):394–395.
- Li W, Cao W, Song H, et al. Recurrent cutaneous necrotizing eosinophilic vasculitis: A case report and review of the literature. Diagn Pathol. 2013 Nov 7;8:185.
- Riyaz N, Sasidharanpillai S, Hazeena C, et al. Recurrent cutaneous eosinophilic vasculitis: A rare entity. Indian J Dermatol. 2016 Mar–Apr;61(2):235.
- Sakuma-Oyama Y, Nishibu A, Oyama N, et al. A case of recurrent cutaneous eosinophilic vasculitis: Successful adjuvant therapy with suplatast tosilate. Br J Dermatol. 2003;149(4):901–903.
- Sawada C, Taniai M, Kawashima M, et al. Recurrent cutaneous eosinophilic vasculitis. Eur J Dermatol. 2016 Jan–Feb;26(1):108–109.
- Sugiyama M, Nozaki Y, Ikoma S, et al. Successful treatment with tacrolimus in a case of the glucocorticoid-dependent recurrent cutaneous eosinophilic vasculitis. Ann Dermatol. 2013 May;25(2):252–254.
- Tanglertsampan C, Tantikun N, Noppakun N, et al. Indomethacin for recurrent cutaneous necrotizing eosinophilic vasculitis. J Med Assoc Thai. 2007 Jun;90(6):1180–1182.
- Tsunemi Y, Saeki H, Ihn H, et al. Recurrent cutaneous eosinophilic vasculitis presenting as annular urticarial plaques. Acta Derm Venereol. 2005;85(4):380–381.
- Crowson AN, Mihm MC Jr, Magro CM. Cutaneous vasculitis: A review. J Cutan Pathol. 2003 Mar;30(3):161–173.
- Venzor J, Lee WL, Huston DP. Urticarial vasculitis. Clin Rev Allergy Immunol. 2002 Oct;23(2):201–216.
- Kano Y, Orihara M, Shiohara T. Cellular and molecular dynamics in exercise-induced urticarial vasculitis lesions. Arch Dermatol. 1998 Jan;134(1):62–67.
- Caputo R, Marzano AV, Vezzoli P, et al. Wells syndrome in adults and children: A report of 19 cases. Arch Dermatol. 2006 Sep;142(9):1157–1161.
- Klion AD. How I treat hypereosinophilic syndromes. Blood. 2009 Oct 29;114(18):3736–3741.
- Quijano-Gomero EG, Rodriguez-Zuniga MJM, Sanz-Montero ME, et al. Clinical, dermoscopic and histologic features of recurrent cutaneous eosinophilic vasculitis cases. Actas Dermosifiliogr. 2018 Jun 21.
- Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013 Jan;65(1):1–11.