After diagnosis, the patient received pulse therapy with glucocorticoids (30 mg/kg/dose = 800 mg) for three days and then transitioned to 20 mg of oral prednisone twice a day, followed by a prednisone wean. She was given rituximab induction therapy (750 mg x two doses, two weeks apart) followed by maintenance therapy (thus far receiving one dose). Currently, she has been weaned off prednisone and is doing well overall, with minimal symptoms.
A follow-up MRI eight months later showed markedly decreased orbital mass, with only a small residual area of enhancement between the right medial rectus and superior oblique muscle. There was also slightly decreased pansinusitis, with osseous destruction of the medial maxillary sinus walls and dehiscence of the right lamina papyracea. Further, the anterior cranial fossa pachymeningeal thickening and enhancement was nearly resolved.
Discussion
Orbital lesions can be caused by a wide range of conditions, including infection, malignancy, foreign bodies, idiopathic or even autoimmune/inflammatory conditions. Those that are caused by inflammatory manifestations are rare in children, but some reports suggest an average onset at about 12 years of age.3,4 In a case series of children with orbital masses, the most common final diagnosis was granulomatosis with polyangiitis.3
Ocular findings in GPA are rarer in children than adults, where they can occur in up to 60% of cases. Reports indicate that up to 16% of adults initially present with orbital inflammatory involvement.5 Orbital GPA can be secondary to extension of sinus disease or isolated inflammation of the orbit itself.6 The most common presenting signs of orbital disease are ptosis, proptosis, pain, blurred vision, eyelid swelling and reduction of eye mobility.
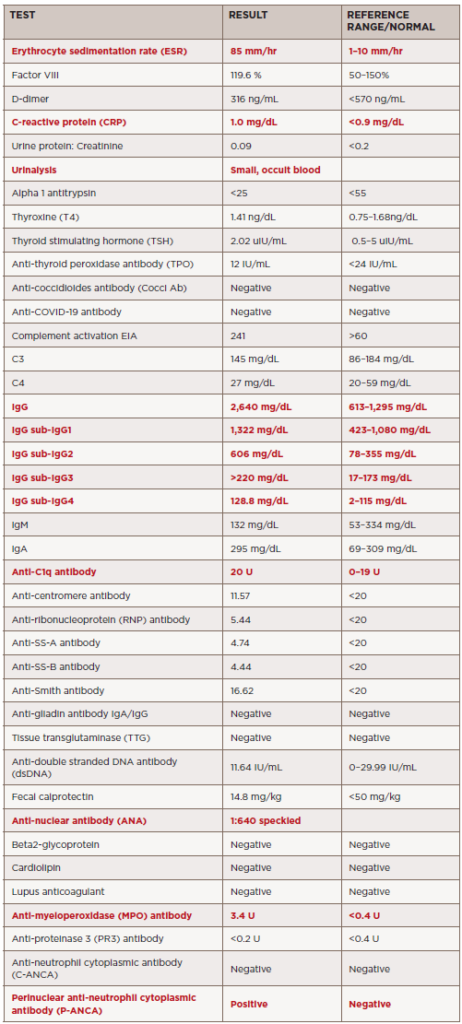
A few case reports have discussed orbital tumors as initial manifestations of GPA in children.7 In one case series, four children presented with unilateral proptosis and ptosis due to an orbital tumor. Further, cases of GPA with orbital mass that can appear like IgG4-related disease have been reported.8 These presentations are strikingly similar to our patient. The tissues from our patient and the case report mentioned above both showed fibrosis with small and medium vessel vasculitis.
Although many of the clinical and radiographic findings are nonspecific for GPA, biopsy in conjunction with these findings can help differentiate this diagnosis from other potential etiologies, including IgG4-related disease. One general histologic finding that may be helpful in suggesting a diagnosis of GPA over other orbital inflammatory diseases is the presence of many scattered eosinophils, particularly eosinophils within granulomas.9