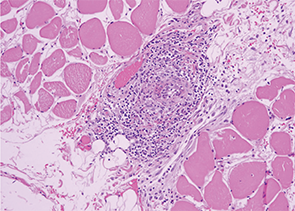
Image 4: The serratus muscle biopsy showed evidence of classic small artery vasculitis.
One week into her steroid treatment, the results of her muscle biopsy returned. Lo and behold, the thoracic surgeon-motivated serratus muscle biopsy showed evidence of classic small artery vasculitis (see Image 4)! Surrounding muscle fibers were variable in size, indicating muscle fiber atrophy secondary to ischemia in the setting of vasculitis (see Image 5). There were no inflammatory infiltrates, perifasicular atrophy or fibrosis, or degenerating or necrotic fibers to suggest inflammatory myositis.
Microscopic Polyangiitis: Unusual Manifestations
Small artery vasculitis on muscle biopsy, along with MPO-ANCA, ILD and constitutional symptoms, clinched the diagnosis of microscopic polyangiitis. Her initial symptoms seemed unusual for MPA; in particular, how were the severe calf and thigh pain part of this disease process? Birnbaum et al reported a case of MPA presenting as a “pulmonary-muscle” syndrome,4 similar to our patient. Common features between that patient and ours included pANCA with elevated MPO, normal CK and aldolase, absence of renal involvement, basilar lung fibrosis on CT chest, and small vessel arteritis identified on muscle biopsy.
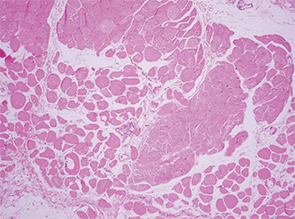
Image 5: Surrounding muscle fibers were variable in size, indicating muscle fiber atrophy secondary to ischemia in the setting of vasculitis.
Calf claudication has also been reported as a presenting symptom of MPA.5 In that case report, the patient had pANCA, elevated MPO and normal PR3, normal CK and bibasilar honeycombing on CT chest. Unlike our patient, the reported case had necrotizing granulomatous vasculitis on muscle biopsy and crescentic glomerulonephritis on renal biopsy.
Summary
The patient’s fever, fatigue, calf and thigh pain, and oxygen desaturation upon walking improved days after starting high-dose steroids, followed by two doses of rituximab 1000 mg IV, two weeks apart. She continues to do well on a steroid taper and prophylactic trimethoprim-sulfamethoxazole.
 Sara Tedeschi, MD, is a rheumatology fellow at Brigham and Women’s Hospital in Boston.
Sara Tedeschi, MD, is a rheumatology fellow at Brigham and Women’s Hospital in Boston.
Acknowledgements: The author thanks Paul Dellaripa, MD, for his assistance in caring for this patient, and Emilian Racila, MD, for the pathology slides.
Key Points
- A small percentage of patients with microscopic polyangiitis have evidence of ILD—rather than small artery vasculitis or capillaritis—on CT scan or lung biopsy.
- A similar, small percentage of patients with idiopathic pulmonary fibrosis have a positive ANCA test at some point in their disease course, and 25% of these may go on to develop microscopic polyangiitis.
- Vascular and interstitial lesions may occur with similar frequency among patients with ANCA vasculitis.
- Muscle biopsy can yield evidence of small vessel arteritis in the setting of ANCA vasculitis.
References
- Arulkumaran N, Periselneris N, Gaskin G, et al. Interstitial lung disease and ANCA-associated vasculitis: A retrospective observational cohort study. Rheumatology. 2011 Nov;50(11):2035–2043.
- Kagiyama N, Takayanagi N, Kanauchi T, et al. Antineutrophil cytoplasmic antibody-positive conversion and microscopic polyangiitis development in patients with idiopathic pulmonary fibrosis. BMJ Open Respiratory Research. 2015 Jan 9;2(1):e000058.
- Gaudin PB, Askin FB, Falk RJ, Jennette JC. The pathologic spectrum of pulmonary lesions in patients with anti-neutrophil cytoplasmic autoantibodies specific for anti-proteinase 3 and anti-myeloperoxidase. Am J Clin Pathol. 1995 Jul;104(1):7–16.
- Birnbaum J, Danoff S, Askin FB, Stone JH. Microscopic polyangiitis presenting as a ‘pulmonary-muscle’ syndrome: Is subclinical alveolar hemorrhage the mechanism of pulmonary fibrosis? Arthritis Rheum. 2007 Jun;56(6):2065–2071.
- Kim MY, Bae SY, Lee M, et al. A case of ANCA-associated vasculitis presenting with calf claudication. Rheumatol Int. 2012 Sep;32(9):2909–2012.

