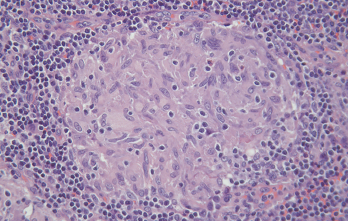
Figure 2. A non-caseating granuloma from mediastinal lymph node biopsy confirming sarcoidosis. H&E magnification x200.
To further characterize the salivary gland enlargement and to evaluate for the possibility of more extensive disease, the patient underwent a PET/CT. These studies showed numerous areas of lymphadenopathy in the cervical chain, axilla, mediastinum and retroperitoneum, measuring up to a maximum of 6.53 standardized uptake values (SUV) and measuring up to 1.2 cm in diameter.
An excisional biopsy of a mediastinal lymph node revealed non-caseating granulomatous changes with negative stains for fungi and acid-fast bacilli (see Figure 2, opposite). This pathology was most consistent with sarcoidosis. Given her medical history of probable IgG4-RD, the specimen was reviewed by a second pathologist internally and also sent for external consultation.
The consensus was for a diagnosis of sarcoidosis, citing the characteristic cellular architecture for sarcoidosis with the presence of non-caseating granulomas and lack of significant numbers of IgG4-positive plasma cells on immunostaining.
The patient was treated for sarcoidosis with glucocorticoids and methotrexate as a steroid-sparing agent. She initially experienced partial relief in the intensity of the urticarial lesions, along with modest improvement in the CRP elevation and reduction in the size of the salivary
gland lymphadenopathy.
With persistent constitutional symptoms of fatigue, ongoing rash and elevated CRP, the patient was started on adalimumab 40 mg subcutaneously every two weeks to help halt the systemic inflammation. However, she did not see significant improvement in her skin changes with the addition of adalimumab, nor was there any decrease of her blood glucose and CRP levels, and the decision to stop the medication was made.
Discussion
Sarcoidosis is an inflammatory disease that can affect any organ system to varying degrees. Although it has been seen in a wide array of populations, it is most commonly reported in Black women, particularly affecting adults under the age of 40 years, and peaking between 20 and 29 years of age.
Patients may report symptoms related to the specific organs involved, and diagnosis must be made on the basis of the encompassing clinical presentation, histological and radiological findings, as well as exclusion of other similarly presenting diseases.
The lungs are most commonly involved, and patients may present with dry cough, dyspnea and chest pain. Imaging classically shows bilateral hilar lymphadenopathy, and pathology shows non-caseating granulomas that can occur in lymph nodes, perivascular sheaths and connective tissue spaces. Because sarcoidosis can mimic several other diseases, it is imperative to rule out other diagnoses, including malignancy, granulomatosis with polyangiitis and infectious causes.1,2
IgG4-RD is a fibroinflammatory disease that, similar to sarcoidosis, can affect nearly any part of the body. Whereas sarcoidosis most often involves the lungs and lymph nodes, IgG4-RD tends to affect the lacrimal glands, salivary glands and pancreas most frequently.
Several markers have been studied in the diagnosis of IgG4-RD, including serum IgG4 levels, plasmablasts and complement levels, which alone are not specific for the diagnosis.3 Histopathology typically demonstrates lesions with elevated IgG4-expressing plasma cells, along with a dense lymphoplasmacytic infiltrate, fibrosis in a storiform pattern and obliterative phlebitis.4
New classification criteria for IgG4-RD were published by the ACR and EULAR in 2019.5 These criteria are composed of three main parts that focus on typical organ involvement, relevant exclusion criteria and sufficient points for classification based on a scoring system that takes clinical, radiologic and histopathologic aspects into account.
Although sarcoidosis and IgG4-RD have some similar characteristics, they remain unique and complex diseases capable of presenting alone or concurrently. Two case reports have been published describing patients presenting with both diseases.
In the first case, an 80-year-old woman presenting with chronic diarrhea and weight loss was found to have pancreatic enlargement on imaging, with evidence of autoimmune pancreatitis on biopsy. Paired with a serum IgG4 concentration of 680 mg/dL (normal: <80 mg/dL), the presentation was strongly supportive of IgG4-RD. Concurrently, a lymph node biopsy showed non-caseating granulomas, consistent with sarcoidosis and inconsistent with IgG4-RD.6
In the second case, a 36-year-old African American man with previously diagnosed sarcoidosis presented with bilateral periorbital swelling. CT imaging showed enlarged lacrimal glands that were then biopsied and histologically supported a diagnosis of IgG4-RD, with findings of dense fibrous tissue, lymphoplasmacytic inflammation and an increased number of IgG4-expressing plasma cells.7
Treatment for sarcoidosis centers on the use of glucocorticoids.1 Conflicting data support the use of methotrexate, hydroxychloroquine or tumor necrosis factor-α (TNF-α) inhibitors for sarcoidosis.8 For IgG4-RD, treatment with glucocorticoids is also first-line therapy. Rituxumab is a preferred treatment for refractory cases, while limited available data suggest the efficacy of immunosuppressive agents, such as azathioprine and mycophenolate.9
In our case, the patient was originally started on prednisone with only partial efficacy. She was started on methotrexate, followed by adalimumab, with the goal of decreasing her systemic inflammatory response from sarcoidosis.
The treatment of IgG4-RD with TNF-α inhibitors has only been reported in case reports, with the hypothesis that a reduction in TNF-α mediated fibrosis may reduce disease activity.
The cases: A 61-year-old woman with IgG4-RD orbital involvement was treated with infliximab, and a 9-year-old girl with IgG4-RD lacrimal gland involvement was treated with adalimumab.10,11 Both of these patients had been resistant to previous therapies. We recommend using the most rigorous classification criteria available to aid in the choice of treatment.
For our patient, the choice of adalimumab treatment after the initial failure of glucocorticoids and methotrexate held the potential to treat both sarcoidosis and IgG4-RD with a medication that was safe and easily discontinued due to its dosing frequency, unlike the irreversible effect of rituximab in depleting B cells. However, after three months of treatment, we did not observe significant changes in her acute phase reactants and the decision to stop treatment was made. The patient deferred further treatment with rituximab.
Because the clinical features of sarcoidosis and IgG4-RD can overlap, a histological diagnosis is critical. This approach also helps rule out other important mimics of the two diseases, such as malignancy or infection.12 There have been limited comparisons of the two diseases at the cellular and cytokine level.
In patients with pulmonary sarcoidosis and IgG4-RD respiratory disease, the bronchoalveloar lavage (BAL) fluid of patients was compared. The cytokine profile of sarcoidosis patients was predominately that of Th1 cytokines with higher levels of interleukin (IL) 2, IL-6 and TNF-α. The IgG4-RD patients had higher levels of Th2 cytokines IL-5 and IL-13.13 These studies demonstrate how far away we stand from the ability to differentiate between IgG4-RD and sarcoidosis with a molecular signature, despite the similar clinical features they may share.
Our case highlights the importance of considering alternative and mimicking diagnoses in patients with a history of IgG4-RD who present with lympha denopathy.