The terrorist attacks on the Twin Towers at the World Trade Center (WTC) that led to their destruction on Sept. 11, 2001, as well as the subsequent year-long cleanup of the site (i.e., Ground Zero) in 2001 and 2002, not only had immediate implications for the lives and health of thousands of individuals at the site, but also caused long-term health effects that continue to be seen in a select group of patients.
We report a case of peritoneal granulomatous disease in a patient thought to have sarcoidosis for over a decade, but which is now believed to be secondary to foreign body exposure from Ground Zero.
The Case
A 50-year-old man who had volunteered at Ground Zero for four months in 2001 presented with abdominal pain in 2022.
He initially developed diffuse, continuous abdominal pain in 2007. Associated symptoms included productive cough with clear sputum and nasal congestion. At that time, laboratory tests were significant for an elevated platelet count of 557×103/μL (reference range [RR]: 150–400×103/μL) and a white blood cell count (WBC) of 11.7×10 3/μL (RR: 4.5–11×103/μL), with neutrophilic predominance. Further testing showed a urine analysis, a basic metabolic panel and creatine kinase were all within normal limits. Testing for infectious causes of his symptoms, including a tuberculosis skin test and blood cultures, was unrevealing.
An X-ray of his chest was unremarkable, but a computed tomography (CT) scan of the abdomen revealed diffuse mesenteric nodules in the peritoneum. An exploratory laparotomy revealed punched-out, noncaseating granulomas, with evidence of focal necrosis, concerning for sarcoidosis or Q fever (Coxiella burnetii infection).
A multi-disciplinary review received from other hospitals concluded the patient likely had either sarcoidosis or Q fever. Kveim testing was negative. The patient was not started on any treatment and was lost to follow-up.
In the following years, the patient continued to experience intermittent episodes of abdominal pain. He did not seek medical care during this time, in part due to frustration with the inability of physicians to offer him a firm diagnosis.
In 2022, he presented to the emergency department with intractable, diffuse abdominal pain, fevers to 102ºF and diaphoresis. He also reported chronic diarrhea and intermittent blurry vision.
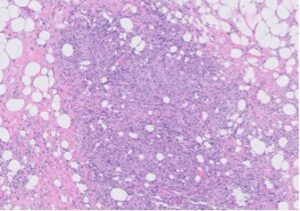
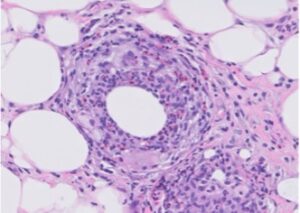
FIGURE 1A: Loose granuloma/swirling histiocytes and admixed acute inflammation can be seen in mesenteric fat. (Click to enlarge.)
A rheumatologist ordered laboratory tests for anti-nuclear antibody (ANA), rheumatoid factor, anti-CCP antibody, SSA/SSB, anti-neutrophil cytoplasmic antibodies (ANCA), myeloperoxidase (MPO) and proteinase (PR3), all of which were normal. Evaluation for HIV, tuberculosis, Strongyloides and Q fever was negative.
Compared with the CT scan of the patient’s abdomen from 2007, the current CT scan revealed ill-defined infiltration of the omentum and mesentery. Diagnostic laparoscopy, lysis of adhesions, omental and small bowel biopsy were performed.
Pathology revealed donut-shaped, non-necrotizing epithelioid granulomas with punched-out central spaces and rare, silver birefringent crystals, atypical for sarcoidosis and more suggestive of a foreign body reaction (see Figures 1A & 1B). The patient was also incidentally found to have elevated liver enzymes. Hepatitis serologies and anti-smooth muscle antibodies were negative. Because his liver enzymes continued to rise, a liver biopsy was performed, and the results were consistent with a nonspecific reactive hepatitis possibly due to a drug reaction unrelated to his granulomatous disease.
Based on these findings, the patient was started on high-dose glucocorticoids and mycophenolate mofetil. His fevers resolved, and the severity of his abdominal pain decreased. He was followed in the clinic, with continued improvement of his symptoms.
Discussion
Asbestos, among other toxic irritants, was found in the dust and air after the WTC collapse. A study of 5,000 Ground Zero rescue workers demonstrated they had an average lung impairment of 10%, based on pulmonary function tests.1 Many individuals who were exposed to the site still experience myriad symptoms, most of which are pulmonary and gastrointestinal.2
Our patient was diagnosed with sarcoidosis in 2008, thought to be related to exposure to the WTC dust at Ground Zero. He continued to develop worsening abdominal pain and constitutional symptoms. However, he did not exhibit any other typical symptoms consistent with sarcoidosis.3 Further, the histopathology of his peritoneum was atypical for sarcoidosis and lacked fibrin rings, which are characteristic of Coxiella burnetii infection. The differentials for granulomatous disease include infectious causes (e.g., tuberculosis) and non-infectious causes (e.g., sarcoidosis, inflammatory bowel disease, hypersensitivity pneumonitis, granulomatosis with polyangiitis).
Vascular-associated granulomas rich in eosinophils can be seen in certain types of hypersensitivity reactions, and the presence of silver birefringent crystals and punched-out granulomas were suggestive of a foreign body. Lastly, although hypersensitivity reactions are heterogenous and may not always respond to glucocorticoids, the resolution of this patient’s symptoms after corticosteroid initiation can be consistent with an inflammatory reaction.
Overall, this case highlights potential issues surrounding individuals who are suffering long-term effects from exposure to the dust at Ground Zero. The patient stated that in the intervening years, he has learned of about 60 of his colleagues from the WTC site who were also diagnosed with sarcoidosis, although we were unable to independently verify this number.
Greater awareness and early detection of diseases from this event may slow the progression of these reactions. Further surveillance among individuals exposed to large quantities of fumes is needed to elucidate the relationship between Ground Zero exposure and granulomatous reactions.
 Branden Ireifej, MD, is a third-year postgraduate internal medicine resident at the Icahn School of Medicine at Mount Sinai, Elmhurst Hospital Center, New York City. He will soon begin his rheumatology fellowship at the University of Southern California, Los Angeles.
Branden Ireifej, MD, is a third-year postgraduate internal medicine resident at the Icahn School of Medicine at Mount Sinai, Elmhurst Hospital Center, New York City. He will soon begin his rheumatology fellowship at the University of Southern California, Los Angeles.
 Lea Meir, MD, is a completing her fellowship in rheumatology at the Icahn School of Medicine at Mount Sinai, New York City.
Lea Meir, MD, is a completing her fellowship in rheumatology at the Icahn School of Medicine at Mount Sinai, New York City.
 Emily Gutowski, MD, is a third-year postgraduate internal medicine resident at the Icahn School of Medicine at Mount Sinai, New York City.
Emily Gutowski, MD, is a third-year postgraduate internal medicine resident at the Icahn School of Medicine at Mount Sinai, New York City.
 Hanson Lam, MD, is a pathologist in the Department of Pathology, Icahn School of Medicine at Mount Sinai, New York City.
Hanson Lam, MD, is a pathologist in the Department of Pathology, Icahn School of Medicine at Mount Sinai, New York City.
 Wei Wei Chi, MD, is an associate professor in the Department of Rheumatology, Icahn School of Medicine at Mount Sinai, New York City.
Wei Wei Chi, MD, is an associate professor in the Department of Rheumatology, Icahn School of Medicine at Mount Sinai, New York City.
References
- Grady D. Lung function of 9/11 rescuers fell, study finds. The New York Times. 2010 Apr 7. https://www.nytimes.com/2010/04/08/nyregion/08lung.html.
- Lippmann M, Cohen MD, Chen LC. Health effects of World Trade Center (WTC) dust: An unprecedented disaster’s inadequate risk management. Crit Rev Toxicol. 2015 Jul;45(6):492–530.
- Srivastava A, Lauwers GY. Pathology of non-infective gastritis. Histopathology. 2007 Jan;50(1):15–29.