He was admitted and placed on contact isolation for suspicion of possible pulmonary tuberculosis. Hematology, infectious diseases and pulmonology subspecialties were consulted.
His condition improved following the infusion of intravenous crystalloids, broad-spectrum antibiotics and nebulization therapy. He was transfused with packed red blood cells and fresh frozen plasma, and was given Vitamin K. On Day 2 of his hospitalization, he underwent fiber-optic bronchoscopy that revealed mild diffuse erythema. Hemorrhagic bronchoalveolar lavage (BAL) fluid was sent for culture, cytology and tests for pneumocystis jirovecii and acid fast bacilli. Results were negative except for a gram stain showing many red blood cells, few white blood cells and no organisms. His respiratory status deteriorated, requiring invasive ventilatory support and critical care. Repeat chest radiograph showed worsening of the the alveolar opacities while his
(click for larger image)
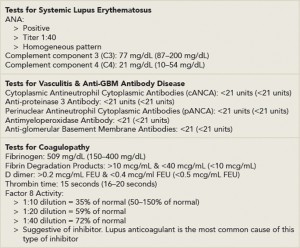
Table 2: Patient Test Results for Systemic Causes of Hemoptysis
*Reference ranges are indicated in parentheses
**FEU = fibrinogen equivalent units
echocardiogram was suggestive of moderate mitral stenosis (valve area 1.5 square centimeters), severe tricuspid regurgitation and severe pulmonary hypertension with pulmonary artery systolic pressure of 74 millimeters of mercury. Computed tomography (CT) of the chest showed extensive alveolar consolidation. His blood and urine cultures were negative for growth.
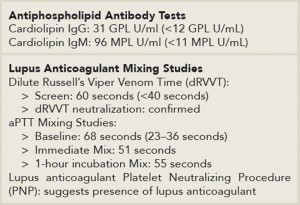
Tests for possible disseminated intravascular coagulation (DIC), microscopic polyarteritis, Churg-Strauss syndrome, antiglomerular basement membrane antibody disease and granulomatosis with polyangiitis were negative (see Table 2). He had positive antinuclear antibody, anticardiolipin immunoglobulin M (IgM) and immunoglobulin G (IgG), elevated dilute Russell’s Viper Venom Time and aPTT mixing studies suggestive of a lupus anticoagulant (see Table 3). There was decreased factor VIII activity, which normalized with 1:20 dilution, also suggesting a lupus anticoagulant. During his hospital stay, it was discovered that he had scheduled foot surgery postponed because of a low platelet count and that he had tested positive for the lupus anticoagulant within the past year. Rheumatology was consulted, and he was started on high-dose corticosteroids.
His platelet count fell to a low of 24,000/cubic millimeters for which he received transfusions of platelets. He subsequently developed generalized tonic-clonic seizures and was started on anti-epileptics. CT of the head showed moderate to large acute infarction involving the left parietal-occipital cortex. He was started on cyclophosphamide and underwent many sessions of plasmapheresis, but continued to deteriorate. He expired 18 days after admission.
(click for larger image)
Table 3: Patient Test Results for Antiphospholipid Antibodies & Lupus Anticoagulant
*Reference ranges are indicated in parentheses
Discussion
For a male presenting with hemoptysis, thrombocytopenia and abnormal coagulation studies, a primarily prothrombotic disorder would not be immediately considered. Differentials for local and systemic disorders that can lead to hemoptysis would be entertained. Potential local causes include bronchopulmonary infections, such as bacterial pneumonia, pulmonary tuberculosis or bronchiectasis, as well as lung cancer, pulmonary edema and pulmonary embolism. Systemic causes, such as hemophilia, or an acquired coagulopathy, such as DIC, which would account for both deranged clotting function and thrombocytopenia, should be considered. In the case of diffuse alveolar hemorrhage, vasculitides, such as granulomatosis with polyangiitis, microscopic polyarteritis and Churg-Strauss syndrome, as well as anti-glomerular basement membrane antibody disease, should be considered.
