ICOS (inducible costimulator on activated T cells) was the first gene defect described in patients with CVID and has so far been described in nine individuals from four families, all of whom inherited the same mutation from a common founder.10 ICOS is expressed on activated T cells and is of critical importance for correct T cell–B cell cooperation during the adaptive immune response. It belongs to the family of T cell co-stimulatory molecules and interacts with ICOS-L on B cells, leading to the release of IL10, IL-17, and several other cytokines from T lymphocytes (See Figure 1A, p. 22). These cellular signals enable B cells to undergo class switch recombination.
In addition to the effects on class switch recombination, ICOS-L/ICOS interactions seem to be crucial for the development of a highly specialized CD4+ T cell subpopulation called follicular T helper cells, which direct the formation of germinal centers in peripheral lymphoid organs.11 ICOS expression loss causes functional germinal center development to fail and therefore leads to impaired terminal B cell differentiation and hypogammaglobulinemia. Childhood onset of the disease was observed in one ICOS-deficient family. All but one adult ICOS-deficient patient had severe peripheral B cell lymphopenia and almost no memory B cells.12
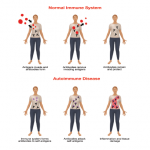
Transmembrane activator and calcium-modulating cyclophilin ligand interactor (TACI) deficiency was the second molecular genetic defect found in patients with CVID.13,14 TACI, which is encoded by the gene TNFRSF13b, is a member of the tumor necrosis factor (TNF) receptor superfamily. TACI interacts with the ligands BAFF/Blys (B cell activating factor, B lymphocyte stimulator) and/or APRIL (A proliferation inducing ligand)—both members of the TNF ligand superfamily. Together with its closest relatives—BAFF-R and BCMA (B cell maturation antigen)—TACI forms a complex signaling network. TACI directs immunoglobulin class switch recombination and negatively regulates B cell homeostasis (See Figure 1B, p. 22). It has been shown that TACI-deficient mouse models develop lymphoproliferation, autoimmunity, and immunodeficiency, a triad reminiscent of the clinical phenotype observed in some CVID patients.
In about 2% to 3% of CVID patients, both TACI alleles are mutated, causing receptor function loss and ultimately resulting in an antibody deficiency. Simple heterozygous TACI mutations are found in up to 8% of CVID patients. These heterozygous changes are believed to act as disease modifiers rather than causing the disease because they are also observed in the normal population, albeit at lower frequencies.15 The clinical spectrum in TACI deficiency is diverse and there is no specific B cell or immunological phenotype. TACI-deficient individuals may be prone to develop lymphoproliferative and autoimmune complications.16 To unravel the genetic complexity and mechanism of particular TACI mutations and to correlate this to the clinical and immunological presentation of TACI-deficient CVID patients is a main research focus for my colleagues and I.