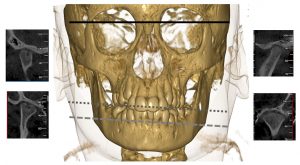
A cone beam CT of an 11-year-old boy with arthritis in the right temporomandibular joint (TMJ). The right TMJ displays deformity with flattening of the condylar head and tuberculum, cortical erosion and a cyst. The left temporomandibular joint has a normal radiographic appearance. There is a notable mandibular asymmetry canting toward the right because of arthritis-induced reduction in facial growth and development in this side (gray reference lines).
Juvenile idiopathic arthritis (JIA) can affect all joints, including the temporomandibular joints (TMJs). For a long time, the TMJ was a “forgotten” joint in pediatric rheumatology, although Sir Frederick Still did comment on a small mandible in his first case series on juvenile arthritis in 1897. In recent years, more attention has been given to the TMJ in JIA; however, the joint is still grossly overlooked in clinical trials and treatment studies due to its difficult-to-assess nature. Orofacial clinical examination recommendations were published in 2017, which will, hopefully, lead to better assessment of this joint in clinical trials and treatment studies.1
The TMJ is a unique joint due to developmental, anatomic and histological properties. In addition, the TMJs perform complex functional movements; the two joints function as one joint during mouth opening. Each TMJ consists of the condyle and the fossa, with an interposed articular disc. The mandibular growth plate is positioned directly underneath the articular surface of the condyle.
Physical damage, such as direct compression or TMJ inflammation, can cause severe mandibular growth disturbances. In patients with JIA, unilateral TMJ involvement can lead to facial asymmetry, and bilateral involvement can lead to retrognathia, the so-called bird-face appearance. Any change in mandibular growth can lead to orofacial signs and symptoms, changes in bite, and therefore, functional and esthetic problems.
In short, TMJ arthritis relates to more than just the jaw joint itself. Signs and symptoms can persist into adulthood and may have a significant impact on general quality of life.2-4
Diagnosis & Challenges
Most patients with JIA-associated TMJ arthritis don’t display symptoms or report any complaints until symptoms cause functional problems and potential damage has occurred. Without consistent, standardized clinical evaluation, the only way to establish the presence of TMJ inflammation is by imaging.
Terminology surrounding JIA-associated TMJ arthritis has been conflicting in the past, making it difficult to compare studies. To enhance collaboration, consensus-based terminology for JIA-related orofacial manifestations were proposed by the Temporomandibular Joint Juvenile Arthritis Working Group (TMJaw; formerly known as euroTMjoint).5 The TMJaw is an international, interdisciplinary network of specialists with a special interest in research and management of TMJ arthritis in JIA.


