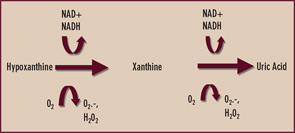
Given the aforementioned limitations of allopurinol, there is interest in selective xanthine oxidase inhibition for hyperuricemia using drugs without a purine-like backbone. One such drug, febuxostat, selectively occupies the substrate access channel to the catalytic site of xanthine oxidase. Significantly, febuxostat inhibits both the reduced and oxidized forms of xanthine oxidase and does not affect interconversion of the enzyme from one form to the other. In a large, randomized, phase III study of gout patients by Michael Becker, MD, and colleagues, febuxostat at doses of 80 and 120 mg daily was more effective than standard dosing (300 mg daily) of allopurinol in reducing serum urate to a target level of less than 6 mg/dL over one year of treatment.5 Febuxostat remains under FDA review, and detailed assessment of febuxostat in patients with renal insufficiency is expected.
A serum urate level of less than 6 mg/dL is widely advocated as an ideal therapeutic target because it is well below the theoretic limit of urate solubility in human tissues of between 6.7 and 7.0 mg/dL, the benchmark provided by in vitro studies in physiologic buffers and plasma. In response to 80 mg and 120 mg of febuxostat daily, the mean drop in serum urate from baseline to the final visit was 44.7% and 51.5%, respectively.5 The majority of allopurinol-treated patients (approximately two-thirds) did not attain sustainable serum urate lowering to less than 6 mg/dL at the final visit.
An important finding in the febuxostat phase III trial was that 300 mg allopurinol daily lowered mean serum urate by a mean of approximately 33%.5 Hence, the average patient with a serum urate of less than or equal to 9 mg/dL should achieve ideal serum-urate lowering with the typical daily dosage of allopurinol. In my experience, higher doses of allopurinol can safely achieve optimal serum-urate lowering in many additional patients. An additional finding in the febuxostat study was that the frequency of gout flares at the end of the study period was comparable in febuxostat- and allopurinol-treated patients, despite the more potent serum-urate lowering by febuxostat. Indeed, serum-urate lowering to less than the “ideal” target level of less than 6.0 mg/dL (but to levels between 6.0 and 6.7 mg/dL) may be sufficient to improve the course of gout in many patients.


