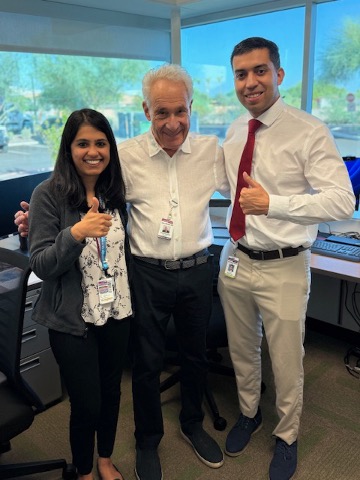
 On July 1, Honor Health in Phoenix launched a new Rheumatology Fellowship Program with two promising fellows. Remarkably, this coincides with the 50th anniversary of the start of my fellowship in Philadelphia, with George E. Ehrlich, MD, and Warren A. Katz, MD.
On July 1, Honor Health in Phoenix launched a new Rheumatology Fellowship Program with two promising fellows. Remarkably, this coincides with the 50th anniversary of the start of my fellowship in Philadelphia, with George E. Ehrlich, MD, and Warren A. Katz, MD.
Where We Started
In my fellowship, I was quickly introduced to detailed information on the diagnosis and treatment of rheumatoid arthritis in a pyramidal hierarchy (i.e., an ancient term for step therapy), with debates regarding the efficacy of parenteral gold vs. the antimalarial hydroxychloroquine, as well as the possibility of a new agent—oral, pulse-dose methotrexate. Discussions included debates on whether to treat such seronegative arthritic conditions as arthritis of psoriasis and HLA-B27-positive ankylosing spondylitis as distinct entities from rheumatoid arthritis.
Among the many questions debated was the categorization of arthritis of enteric inflammatory conditions, as well as reactive arthritis. Was Sjögren’s disease a secondary condition? Were non-steroidal anti-inflammatory drugs better than dosing aspirin (which we played by ear)? Azathioprine was thought to be a monotherapy superior to, and perhaps safer than, maintenance corticosteroid for lupus nephritis. Scleroderma left us frustrated, although eminent rheumatologist Gerald P. Rodnan, MD, an expert in this field, was hopeful. Juvenile rheumatoid arthritis was becoming known as chronic juvenile arthritis.
In addition, questions arose about how best to treat osteoarthritis. The spectrum of vasculitis was classified by vessel type and size, as well as laboratory testing. Anti-nuclear antibody testing showed promise to improve sensitivity over lupus erythematosus cell prep for the diagnosis of systemic lupus erythematosus. Fibrositis was used to describe enigmatic chronic pain. Anthony Bohan, MD, and James B. Peter, MD, PhD, were classifying polymyositis. Of course, did we ever use prednisone.
The decades brought exciting and promising changes as the American Rheumatism Association became the American College of Rheumatology. Aggressive diagnostic treatments of early and established rheumatoid arthritis employed advances in immunology, genetics, imaging and pharmacology, as well as clinical-metric yielding improved benefit and prognosis. Now, we addressed preclinical rheumatoid arthritis. As Daniel J. McCarty, MD, once famously suggested, we could suppress rheumatoid inflammation early and leave the pyramid to the Egyptians.
Lumpers and splitters still discuss the similarities and distinctions of seronegative arthritis, with sharper metrics and diagnostic and therapeutic modalities. The totality of systemic lupus is unfolding, with refining classification, diagnostic and therapeutic approaches. Juvenile chronic arthritis is now known as juvenile idiopathic arthritis, with subtypes and more precise treatments. Better understanding of the scope of vasculitis, as well as its mimics, yields keener diagnostic skills and selective treatments.