Her clinical phenotype was suggestive of an autoinflammatory disease, so she was referred to our Center of Autoinflammatory Diseases for further workup. Due to the gastrointestinal symptoms, repeat colonoscopy showed only sigmoid diverticulosis.
Genetic testing by Next-Generation Sequencing for periodic fever panel of five genes (familial Mediterranean fever, cryopyrin-associated periodic fever syndrome, TNF-receptor-associated periodic syndrome, hyper-IgD syndrome and NOD2) detected two heterozygous variants in the NOD2 gene (IVS8+158 and 1007FS). The patient was initiated on sulfasalazine.
Discussion
Yao syndrome (YAOS, OMIM 617321), formerly called NOD2-associated autoinflammatory disease, is an autoinflammatory disease characterized by periodic fever, dermatitis, arthritis and swelling of the distal extremities, as well as gastrointestinal and sicca-like symptoms (see Figure 2, p. 44). The disorder is associated with specific NOD2 variants. YAOS is a multi-organ polygenic systemic disease and can also cause recurrent oral ulcers, pleuritis, pericarditis, lymphadenopathy, sore throat and ocular myositis. It occurs in the Caucasian population with female-to-male ratio of 2:1. Acute-phase reactants are often elevated.
YAOS differs from inflammatory bowel disease, Blau syndrome, primary Sjögren’s syndrome and monogenic hereditary systemic autoinflammatory diseases.1-3
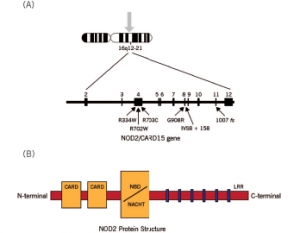
Figure 3. Schematic diagram of the NOD2 gene graph and protein structure.
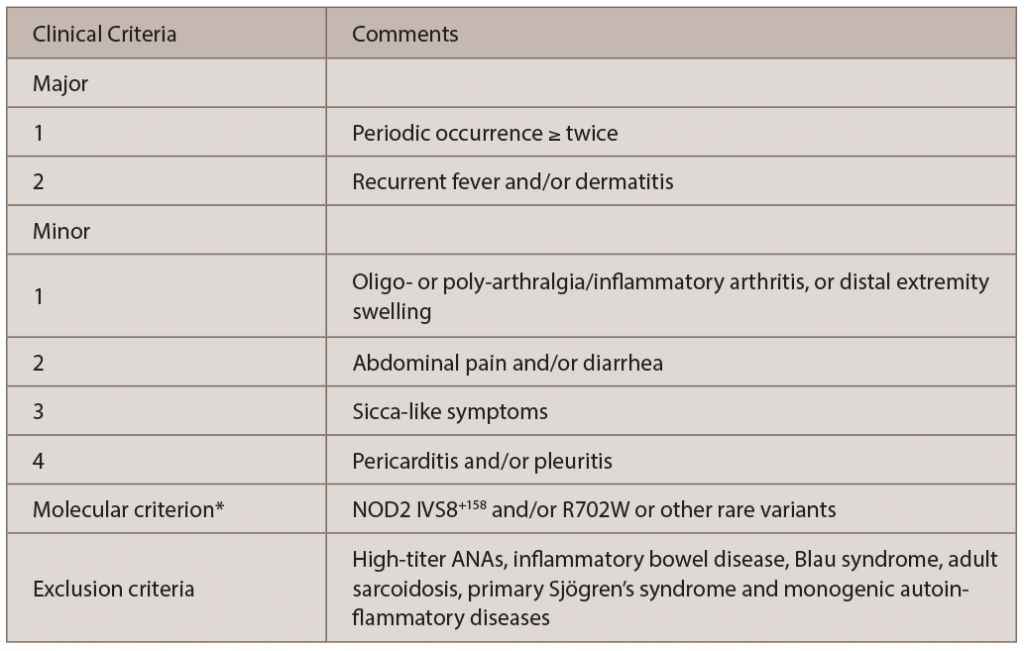
The diagnosis of YAOS is dependent on the characteristic phenotype and genotype, as well as exclusion criteria (see Table 1).4 Our patient presented with typical clinical phenotype and genotype, consistent with YAOS by the diagnostic criteria.
Susceptibility to YAOS is conferred by variation in the NOD2 gene on chromosome 16q12-21 (see Figure 3).3 Genetic testing for NOD2 variants is an integral part of the disease diagnosis. The most frequent variant seen in YAOS is NOD2 IVS8+158, and up to 25% of patients can have concurrent R702W. Other NOD2 rare variants can be seen also.
Therapeutic regimen for YAOS consists of glucocorticoids and/or sulfasalazine in general. For refractory symptoms, both IL-1 and IL-6 antagonists, such as canakinumab and tocilizumab, can be tried with effectiveness in some cases. As a systemic inflammatory disease, YAOS can involve multiple organs, but with rare influence on the internal solid organs. It can cause chronic pain syndrome, fibromyalgia and even disability in some cases. Relatively common comorbidities are fibromyalgia, asthma and urinary stones as in our case.4 YAOS is relatively common when compared with monogenic systemic autoinflammatory diseases in the American adult patient population.5
The prevalence of YAOS has been estimated to be 1 to 10/100,000.3 Other medical institutions have seen or reported cases of the disease.6 Early and prompt recognition of the disease can minimize duplication of extensive and expensive testing, and with a correct diagnosis, physicians are able to manage the patients with assurance.