The CSF analysis of patients with NMOSD is variable. White blood cell counts in CSF are frequently normal or only minimally elevated; however, very high cell counts above 100/uL similar to our patient have been described.2 The presence of neutrophils or eosinophils greater than 5/uL argues in favor of NMOSD over MS. The lack of oligoclonal bands is supportive of the diagnosis because it is seen in less than 20% of patients with NMOSD; however, they can be transiently noted during an attack.
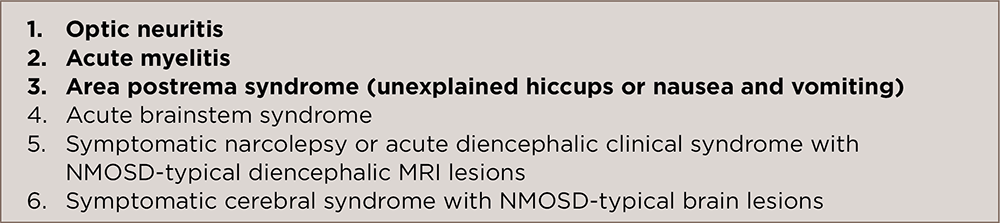
In 2015, a revised international consensus criteria for the diagnosis of NMOSD proposed by the American Academy of Neurology included criteria using the results of testing for AQP4-IgG.2 The diagnostic criteria state the patient should demonstrate at least one other core clinical characteristic (see Table 1) if AQP4-IgG is positive. If AQP4-IgG is negative or unknown, then the patient should have at least two core clinical characteristics, with one of them being among the first three characteristics mentioned in Table 1.
(click for larger image)
TABLE 1: Core Clinical Characteristics for NMOSD
If AQP4-IgG is positive, then the patient must exhibit one of the six clinical characteristics listed. If AQP4-IgG is negative or unknown, two clinical features are required, but one must be a characteristic identified in bold. Adapted from Wingerchuk et al. 2015. Ref. No. 2.
In addition, it is imperative to exclude alternative diagnoses, such as infection, malignancy, MS and sarcoidosis. This is especially important to consider in situations in which the clinical presentation demonstrates a more gradual neurologic course with clinical worsening otherwise not related to attacks; when the CSF analysis demonstrates oligoclonal bands; when there are imaging features more typical of MS. The expected MRI findings of optic neuritis demonstrate increased signal in the optic nerve on T2-weighted images, with fat suppression, with gadolinium enhancement seen on T1.
NMOSD can be related to other autoimmune/rheumatologic conditions, as well. It is estimated that 30–50% of NMOSD patients have laboratory or clinical evidence of these diseases.1 One retrospective study conducted at the Mayo Clinic evaluated 153 U.S. patients with NMOSD and found that there was coexisting autoimmune disease in 62 (40.5%) of the patients—autoimmune thyroid disease (17%), ulcerative colitis (2.6%), SLE (2%), Sjögren’s syndrome (2%), rheumatoid arthritis (1.3%), myasthenia gravis (1.3%) and idiopathic thrombocytopenic purpura (1.3%), among others.3 Because some of these conditions, such as SLE, may cause visual loss, one should carefully evaluate patients to rule out the diagnostic possibilities, especially in those patients who are negative for AQP4-IgG.
NMOSDs, also known as Devic disease, are autoinflammatory, demyelinating conditions affecting the central nervous system. The pathogenesis is thought to be directly linked to the highly specific Aquaporin-4 antibody (AQP4-IgG), which targets the water channel most common in astrocytes.
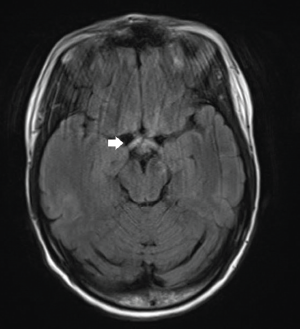
FLAIR sequence demonstrates increased signal in the optic chiasm and proximal optic radiations, as well as optic nerves.



