B cell depletion with rituximab may improve symptoms, but not reverse fibrosis on imaging, he said. “Nevertheless, patients’ lives can be improved enormously by treatment, so with either steroids and/or rituximab, we should be aggressive.”
Eosinophilic Fasciitis
Eosinophilic fasciitis (EF) is a very rare, fibrotic disease that may mimic scleroderma. Look for key signs to make the right diagnosis, said Alisa N. Femia, MD, a dermatologist at New York University Langone Medical Center. In EF, fibrosis of the fascia can lead to contractures and functional impairment. Despite misconceptions, EF can involve the hands and feet, she said.
“Patients may come in with a scleroderma diagnosis and thickened skin, but in EF, nailfold capillary changes and Raynaud’s phenomenon are typically absent, and if Raynaud’s is present, it is not likely to be severe. In addition, in EF, the distal digits are spared,” said Dr. Femia. Other signs of EF are the groove sign, or linear furrowing along the venous structures, and pseudocellulitic appearance of the skin. In a new study of EF, 37 of 47 patients were originally misdiagnosed with such disorders as systemic sclerosis, cellulitis, deep-vein thrombosis or hypereosinophilic syndrome.3
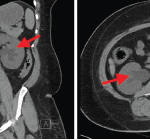
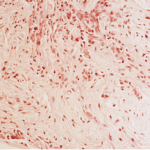
Clinical diagnosis of EF has been made by fascial biopsy showing fibrosis of the fascia, as well as a mixed inflammatory infiltrate of lymphocytes, plasma cells and, at times, eosinophils, but “now, we are moving more toward diagnosis with MRI, which may have the benefit of identifying an appropriate site for biopsy and helping you follow your patient’s disease course,” said Dr. Femia. EF patients may have localized plaque morphea. New research indicates EF patients may have increased expression of Th1 and Th17 cells as well.
Prednisone was effective in a 1988 study of 52 EF patients, but relapse after therapy is a concern, she said.4 Later research suggests a combination of prednisone and disease-modifying antirheumatic drugs, such as methotrexate, successfully treats EF. Mycophenolate mofetil in combination with steroids may be helpful for patients who are not candidates for or cannot tolerate methotrexate. “Always prescribe treatment in combination with physical therapy as soon as the patient feels well enough to do it,” said Dr. Femia.
Scleredema & Scleromyxedema
Two scleroderma mimics so rare that they have no ICD-10 codes, scleredema and scleromyxedema, have notable signs that help confirm diagnosis, said Laura K. Hummers, MD, ScM, co-director of the Johns Hopkins Scleroderma Center in Baltimore.5
“All scleroderma mimics are not primarily fibrotic. What we see in scleredema and scleromyxedema are that these are mucinous deposition disorders. The primary problem in the skin is not necessarily collagen,” said Dr. Hummers.6 Mucin is a protein typically secreted from the epithelial cells that becomes very highly glycosylated and “gummy,” with a high molecular weight. Dermal mucin is composed of acidic glycosaminoglycans, most commonly hyaluronic acid, and produced by dermal fibroblasts.