Kamon_Wongnon / shutterstock.com
The adage frequently cited in healthcare settings, “If it isn’t documented, it wasn’t done,” still rings true for the key components required in a patient’s medical record. The note in the medical record must sufficiently describe all of the services furnished to patients on a specific date.
The essential requirements to appropriately bill a claim and ultimately have it properly adjudicated involve reasonable documentation that the service(s) validate the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided.
The examination usually occurs after the provider obtains the chief complaint and history of present illness—the reason the patient is in the office, whether it’s a follow-up visit or to address an acute problem. Because the examination will be dictated by the patient’s complaint, it is safe to assume the exam could involve a single organ system, several organs and/or several areas. For example, if a patient presents with elbow pain, the provider would focus predominantly on examining the elbow and the arm to determine the extent of the paint. This enables the provider to base his/her judgment on what these findings are and how to treat. Keep in mind that one area of concern does not necessarily require a complete head-to-toe exam and should be determined on the basis of the findings. A head-to-toe examination is just that, depending on the severity of symptoms presented. A comprehensive exam requires a head-to-toe examination of the ears, eyes, nose, abdomen and extremities. All exams would need to be performed and documented.
Unlike the components of history and medical decision making, the rules defining the various levels of physical exam differ; two sets of guidelines exist—those from 1995 and those from 1997. The 1995 evaluation and management (E/M) guidelines allow the physician to complete the physical exam by documenting organ systems or body areas, which can be subjective but allows providers more leeway and “wiggle room.” On the other hand, the 1997 E/M guidelines are relatively rigid and force providers to document using more specificity through a bullet system. But the 1997 examination rules are much more black and white—either the bullets are there or they aren’t.
The levels of E/M services are based on four types of examination defined as follows:
- Problem Focused—A limited examination of the affected body area or organ system.
- Expanded Problem Focused—A limited examination of the affected body area or organ system and other symptomatic or related organ system(s).
- Detailed—An extended examination of the affected body area(s) and other symptomatic or related organ system(s).
- Comprehensive—A general multisystem examination or complete examination of a single organ system.
1995 E/M Guidelines Examination Rules
For the purpose of documenting an examination using the 1995 guidelines, the following body areas are recognized:
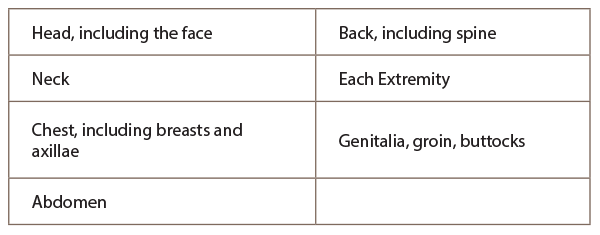
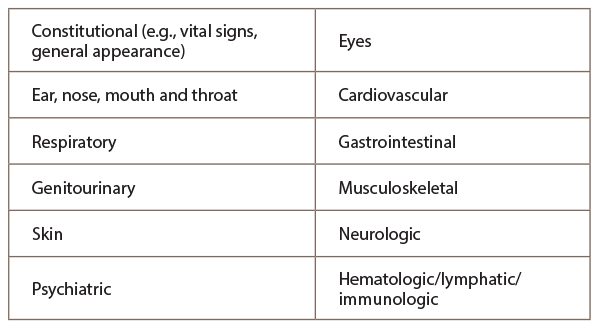
And the following organ systems are recognized:
To appropriately document for the 1997 E/M examination guidelines, it’s important to note this set of physical examinations consists of the general multisystem exam or the single organ (specialty) exam, and each relies on the use of bullets from distinct organ systems:
- Problem Focused—One to five bullets from one or more organ systems.
- Expanded Problem Focused—At least six bullets from any organ systems.
- Detailed—At least two bullets from six organ systems or 12 bullets from two or more organ systems.
- Comprehensive—Two bullets from each of nine organ systems.
A comprehensive exam requires a head-to-toe examination of the ears, eyes, nose, abdomen & extremities. All exams would need to be performed & documented.
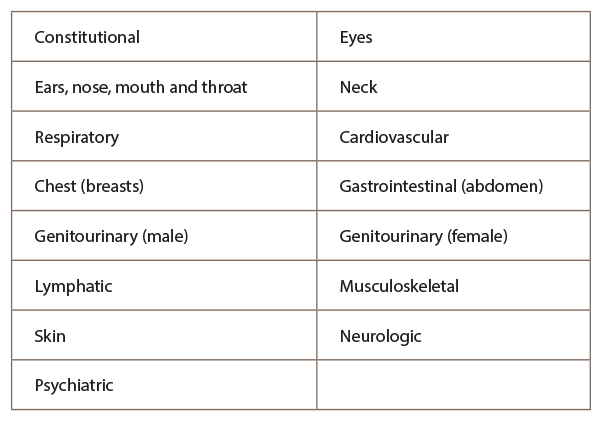
The 1997 E/M guidelines recognize the following organ systems:
The extent of examinations performed and documented depends on the provider’s clinical judgment and the nature of the presenting problem(s). They range from limited examinations of single body areas to general multisystem or complete single organ system examinations. The Centers for Medicare & Medicaid Services (CMS) has documentation guidelines (DG) for what it wants in the patient chart(s) including, but not limited to:
- DG: Specific abnormal and relevant negative findings of the examination of the affected or symptomatic body area(s) or organ system(s) should be documented. A notation of abnormal without elaboration is insufficient.
- DG: Abnormal or unexpected findings of the examination of the unaffected or asymptomatic body area(s) or organ system(s) should be described.
- DG: A brief statement or notation indicating “negative” or “normal” is sufficient to document normal findings related to unaffected area(s) or asymptomatic organ system(s).
- DG: The medical record for a general multisystem examination should include findings about eight or more of the 12 organ systems.
The physical examination is just another component of the evaluation and management visit required to communicate among healthcare professionals evidence of patient care, as well as justifying billing for a claim. Practices are providing patients with quality care, as well as providing information documentation to ensure accurate and timely reimbursement for the services rendered to patients.
The outline provides the core pieces to document properly for the physical examination in E/M coding education. For more information on simplifying the Medicare and private payer coding guidelines to help ensure accurate reimbursement, contact the ACR coding and auditing specialists at [email protected].