Another approach: Taper 60 mg of prednisone over two to three months to a daily dose equivalent of between 2.5 and 10.0 mg/d of prednisone and then maintain this dose for several years.47 IgG4-TIN, even in cases with severe interstitial fibrosis, shows a brisk response to steroids (see Table 7). Although IgG4-RD shows a rapid response to steroids, the disease may recur after steroid tapering or withdrawal.48
In a cohort of 14 patients with no renal impairment (eGFR >60 mL/min/1.73 m2) but with imaging abnormalities, treatment with glucocorticoids improved the imaging abnormalities without a change in eGFR after a mean follow-up period of 42.4 ±17.0 months. Data from the same cohort indicated that 20% of patients treated with glucocorticoids experienced a relapse while on maintenance therapy (prednisolone median 5 mg daily), with a mean follow-up period of only 44 months.49 The natural course of IgG4-related TIN without treatment remains unknown. If a nontreatment strategy is chosen, close observation of renal function is warranted. Renal atrophy may occur in many patients with IgG-4-related TIN, and thus, treatment without overt clinical renal impairment is reasonable.
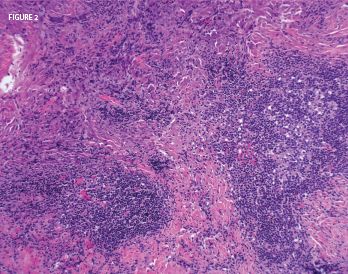
Figure 2: A nasal biopsy of a mass lesion showed lymphoid aggregates (abundant plasma cells) and dense fibrosis. Histopathologic image courtesy of Dr. Paul Cohen, Yale University.
In a study conducted by Quattrocchio et al., one patient with IgG4-RTIN was treated with steroids and rituximab, and four patients (two with IgG4-RTIN and two with IgG4-related RF) were treated with the following immune suppressive protocol for severe systemic lupus erythematosus nephritis: three pulses of 15 mg/kg intravenous methylprednisolone followed by oral tapering of prednisone plus two pulses of 500 mg intravenous cyclophosphamide (on days 1 and 15), plus four weekly rituximab administrations at 375 mg/m2. Two more doses of rituximab were administered one and two months after the last weekly infusion. Renal function improvement was observed in all patients (see Table 7).50
Experience with treating MGN associated with IgG4-RD was derived from a retrospective analysis of seven patients with a mean follow-up period of 39 months (ranging from 4–184 months). Four of those patients had concomitant biopsy proven IgG4-related TIN. Treatment of those seven patients varied: Two patients received prednisone; two initially were treated with prednisone alone and subsequently received prednisone with MMF; one received prednisone, cyclophosphamide and an angiotensin-converting-enzyme inhibitor (ACE-I); one received an ACE-I followed by rituximab and mycophenolate mofetil (MMF); and one patient went untreated (see Table 7). Data revealed a decline in proteinuria from a mean baseline of 8.8 g daily (3.5–16 g daily) to 1.2 g daily (ranging from 0–3.1 g daily) and an improvement in the mean serum creatinine concentration from 221.0 μmol/L (ranging from 70.7–583.4 μmol/L) to 123.8 μmol/L (ranging from 70.7–583.4 μmol/L).5