BIOPHOTO ASSOCIATES / SCIENCE SOURCE
EULAR 2022 (VIRTUAL)—For years, the gold standard for gout diagnosis has been the presence of monosodium urate (MSU) crystals on synovial fluid analysis. But any practicing rheumatologist can tell you that tapping a joint isn’t always feasible. And any patient with a red, hot, swollen joint can tell you that having a needle stuck into that joint isn’t always preferable. Fortunately, imaging is becoming more and more a part of day-to-day gout diagnosis and treatment.
At the 2022 Congress of the European Alliance of Associations for Rheumatology (EULAR), Tristan Pascart, MD, PhD, full professor of rheumatology, Université Catholique de Lille, France, provided evidence-based, practical insight into the use of gout imaging modalities in clinical practice.
Diagnosis
In 2015, the ACR and EULAR published classification criteria for gout via a collaborative initiative.1 The presence of MSU crystals in a symptomatic joint, bursa or tophus was a sufficient criterion for classification as gout. If crystal analysis isn’t available, a patient could be classified as having gout via a combination of clinical, laboratory and imaging findings.
However, the criteria aren’t 100% sensitive or specific, synovial fluid analysis is invasive and often unavailable, and radiographic gout findings come too late. Additionally, Dr. Pascart noted that “clinical exam and serum urate levels don’t reflect the crystal burden in joints, which is why patients flare even after serum urate levels are at goal.”
Dual-energy computed tomography (DECT) and ultrasound are both more sensitive than plain radiographs and provide noninvasive characterization of MSU crystals with specificity. “This is why imaging findings account for half of the points you need to classify a patient as gout by the ACR/ EULAR criteria,” Dr. Pascart explained.
Ultrasound
When it comes to ultrasound, the two most important and reliable diagnostic features to look for are the double contour sign and tophi. Both are quite specific for MSU crystals. On the other hand, hyperechoic aggregates have poor inter-observer reliability and insufficient specificity.2,3 “I wouldn’t rely on aggregates alone,” Dr. Pascart cautioned.
Ultrasound is also useful as a semiquantitative tool for monitoring response to treatment. The thickness of the double contour sign can be measured over time. The double contour sign is the ultrasonographic finding that’s most sensitive to change.4
Like any test, ultrasound has its drawbacks. Dr. Pascart explained, “Ultrasound is observer dependent, and most, if not all, of the data on the diagnostic performance of ultrasound come from expert hands. So we don’t really know what happens when less expert people do it.”
DECT
When it comes to dual-energy computed tomography, Dr. Pascart noted that “diagnostic accuracy is a bit better for DECT than ultrasound, with the exception of early disease.” In early disease (i.e., diagnosis of gout within the first two years of disease onset), ultrasound is more sensitive for new deposits as appreciated by the double contour sign.5 This is because DECT is limited by resolution. Significant MSU crystal aggregates need to be present to see them.
It’s also important to make sure that radiologists aren’t counting artifact while calculating MSU crystal burden on DECT images. “Nailbeds have the same signature as MSU crystals and shouldn’t be counted. Metal implants can also cause artifact,” Dr. Pascart explained.
“I like to use DECT for prognosis and follow-up,” Dr. Pascart said, “but I do admit I’m a bit biased since it’s so cool. We know there’s a relationship between the volume of crystals measured with DECT at baseline and flare risk over the next six months.6 With ultrasound, after six months of treatment, patients with a greater than 50% decrease in tophus size had less risk of flaring after those six months of treatment.7 [Given this information], you might argue for a lower serum urate target or prolonged flare prophylaxis if tophus burden as measured by DECT remains high.”
Dual-energy computed tomography & ultrasound are both more sensitive than plain radiographs & provide noninvasive characterization of monosodium urate crystals with specificity.
Ultrasound & DECT
What about using ultrasound and DECT in combination? Dr. Pascart et al. used prospectively collected data from an outpatient rheumatology clinic to examine the diagnostic accuracy of either modality alone or in combination, by anatomical site (i.e., feet and ankles, and knees).5 “The general conclusion,” Dr. Pascart explained, “was that there was no advantage to combining the two techniques. You gained some sensitivity but lost some specificity.”
In Sum
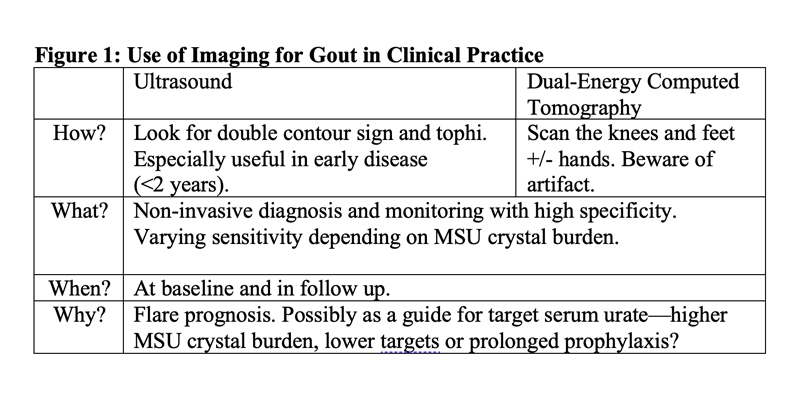
Dr. Pascart concluded his talk with a highyield summary of the “how, what, when and why” of imaging modalities in gout (see Figure 1, below). As ultrasound and DECT become more widely available, we can all hope for better care of our gout patients in the future.
Samantha C. Shapiro, MD, is an academic rheumatologist and an affiliate faculty member of the Dell Medical School at the University of Texas at Austin. She is also a member of the ACR Insurance Subcommittee.
References
- Neogi T, Jansen TLTA, Dalbeth N, et al. 2015 gout classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheumatol. 2015 Oct;67(10):2557–2568.
- Terslev L, Gutierrez M, Schmidt WA, et al. Ultrasound as an outcome measure in gout. A validation process by the OMERACT Ultrasound Working Group. J Rheumatol. 2015 Nov;42(11):2177–2181.
- Christiansen SN, Filippou G, Scirè CA, et al. Consensus-based semi-quantitative ultrasound scoring system for gout lesions: Results of an OMERACT Delphi process and web-reliability exercise. Sem Arthritis Rheumatol. 2021 Jun;51(3):644–649.
- Hammer HB, Karoliussen L, Terslev L, et al. Ultrasound shows rapid reduction of crystal depositions during a treat-to-target approach in gout patients: 12-month results from the NOR-Gout study. Ann Rheum Dis. 2020 Nov;79(11):1500–1505.
- Singh JA, Budzik JF, Becce F, Pascart T. Dual-energy computed tomography vs ultrasound, alone or combined, for the diagnosis of gout: A prospective study of accuracy. Rheumatology (Oxford). 2021 Oct 2;60(10):4861–4867.
- Pascart T, Grandjean A, Capon B, et al. Monosodium urate burden assessed with dual-energy computed tomography predicts the risk of flares in gout: A 12-month observational study: MSU burden and risk of gout flare. Arthritis Res Ther. 2018 Sep 17;20(1):210.
- Ebstein E, Forien M, Norkuviene E, et al. UltraSound evaluation in follow-up of urate-lowering therapy in gout phase 2 (USEFUL-2): Duration of flare prophylaxis. Joint Bone Spine. 2020 Dec;87(6):647–651.