The patient reported he developed COVID-19 and recovered well. One month later, he developed sharp burning pain, numbness and weakness in both of his arms and legs. His rheumatologist was concerned and sent an initial request for an evaluation of polyneuropathy and messaged the neuro-rheumatologist for urgent referral.
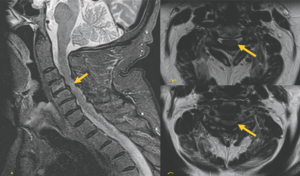
FIGURE 1 (Click to enlarge.)
Left: T2 STIR Sagittal MRI shows multi-degenerative disc disease with severe stenosis and abnormal cord signal at C4-C5.
[mobile-ad name="Advert 1"]Top right: Axial T2 at the C3-C4 level shows posterior disc osteophyte complex effacing the majority of the CSF space.
Bottom right: Axial T2 at the C4-C5 Posterior disc osteophyte complex, which effaces the ventral CSF space that contacts and deforms the spinal cord and ligamentum flavum buckling.
Due to the embedded nature of the clinic and rapidly worsening walking, the patient was added to the neurologist’s schedule two weeks later. At his neurology visit, additional screening revealed he had severe neck pain and intermittent bowel and bladder incontinence. His exam was notable for reduced strength in both arms, distally more than proximally; reduced strength at both hips; brisk reflexes, with the exception of the ankles, which were reduced; and a sensory exam notable for reduced sensation at the great toes and hands.
Based on the exam, with sensory loss in a non-dermatomal or length-dependent distribution and additional neck pain and bowel and bladder involvement, a myelopathy superimposed on a peripheral neuropathy was suspected. The patient was sent for urgent spinal imaging, which showed severe spinal stenosis with abnormal cord signal (see Figure 1).
He was referred urgently to neurosurgery and underwent C2-5 laminectomy and medical fasciotomy. At follow-up one month later he had recovered his ability to perform activities of daily living including buttoning his shirt and using his computer. He also regained strength in his legs and was able to use a walker.
 Kristin Galetta, MD, is an instructor of neurology in the Department of Neurology, Brigham and Women’s Hospital and Harvard Medical School, Boston.
Kristin Galetta, MD, is an instructor of neurology in the Department of Neurology, Brigham and Women’s Hospital and Harvard Medical School, Boston.
 Shamik Bhattacharyya, MD, is an assistant professor in the Department of Neurology, Harvard Medical School, Boston.
Shamik Bhattacharyya, MD, is an assistant professor in the Department of Neurology, Harvard Medical School, Boston.

Dr. Helfgott
Simon M. Helfgott, MD, is an associate professor of medicine in the Division of Rheumatology, Immunology and Allergy at Harvard Medical School, Boston, and a previous physician editor of The Rheumatologist.
Disclosures
Dr. Galetta has received personal compensation for consulting from Glaxo Smith Kline.