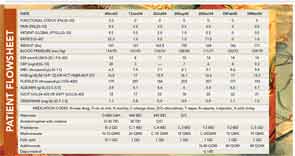
An example of a person with RA who was treated with prednisone 3 mg/day and methotrexate 10 mg/week is presented in a flow sheet from actual care (see Figure 2) The patient initially self-reported scores for physical function of 3.3 (0–10), pain 9.5 (0–10), global status 9.5 (0–10), and a RAPID3 score of 22.3 (0–30), indicating high severity (>12). Two months after initiation of prednisone 3 mg/day and methotrexate 10 mg/week, his RAPID3 score was 1, indicating near-remission. He was stable over a year, but experienced a severe flare 13 months after initial presentation, with a RAPID3 score of 11.5, at the upper limit of moderate severity (6–12). After lengthy discussion with the patient and his family, he chose to be treated with adalimumab and an intramuscular injection of 40 mg methylprednisone. Two months later, all his scores were 0. Throughout this period, his daily prednisone dose was maintained at 3 mg/day although, as noted, he was given an intramuscular injection at the time of a severe flare.
The case for treatment with prednisone in doses of 5 mg/day or less includes:
