An Unforgettable Story
Her name was unforgettable. Not only did we share our given names—Simon and Simone, but her French-Canadian surname was based on this appellation, too. I was the junior resident working on our hospital’s nephrology service when she was admitted for evaluation of progressively worsening kidney disease and an overall failure to thrive. A single woman in her early 50s, she had recently moved in with relatives who had observed with growing alarm her steady decline in health. She had no appetite and had lost a considerable amount of weight. She became a recluse, rarely venturing outdoors to shop or visit friends.
She seemed to have one complaint that rose far above the others: She was constipated. Terribly constipated. As her cousin described it, it became her one and only focus. No conversation with Simone was ever complete without a discussion of her constipation. Enemas, laxatives and all forms of purges failed to move her bowels. She recounted how she had undergone a barium enema weeks earlier and not only had it failed to provide any answers, the barium made her constipation even worse! There remained no other option but to admit Simone to hospital.
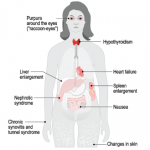
A cursory set of lab tests ordered in the emergency department provided a few clues: Anemia, elevated creatinine and frothy urine signified a heavy degree of protein loss. Unlike our current system, in which the average inpatient length of stay is often measured in hours, this was the predigital era, when the pace was slower and patients could spend days or weeks wandering and wondering on the ward as their doctors trudged steadily toward a diagnosis. I got to know Simone well as our team worked to untangle her disparate issues—the kidney disease, the constipation and the baffling observation that she had no arterial pulses to be felt anywhere.
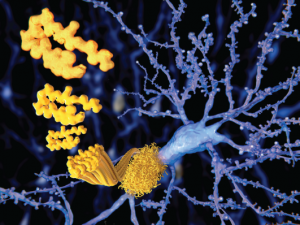
The beta amyloid peptid, amyloid plaques growing on a neuron.
Juan Gaertner / Shutterstock.com
We identified some interesting clues, including a thickened tongue that seemed to get in the way of her speaking fluently, a peripheral neuropathy that explained her reluctance to venture too far from her bed and many, many bruises that would spontaneously erupt over her waxy skin.
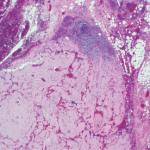
We were closing in on the diagnosis. We had a suspicion that an infiltrative disorder could explain her multisystem demise. A skin and fat pad biopsy was planned for the following day. But it never happened: That evening, Simone was found dead in her bed. A sudden death.