Patients with Takayasu’s arteritis (TA) have an increased risk for stroke. Approximately 16% of individuals diagnosed with TA experience a stroke and its resulting disability. Due to this risk, physicians typically treat patients with TA with low-dose aspirin, as well as anti-inflammatory medications, such as corticosteroids and immunosuppressive drugs. Although the incidence of stroke and ischemic stroke in these patients has been documented, the underlying mechanism remains unclear. Researchers have noted that the patients at greatest risk for stroke tend to have a dual diagnosis of antiphospholipid syndrome and/or the presence of lupus anticoagulant. Additionally, patients with TA who also have anemia and low body mass index (BMI) appear to be at greater risk of cardiovascular disease.
Patients with Takayasu’s arteritis (TA) have an increased risk for stroke. Approximately 16% of individuals diagnosed with TA experience a stroke and its resulting disability. Due to this risk, physicians typically treat patients with TA with low-dose aspirin, as well as anti-inflammatory medications, such as corticosteroids and immunosuppressive drugs. Although the incidence of stroke and ischemic stroke in these patients has been documented, the underlying mechanism remains unclear. Researchers have noted that the patients at greatest risk for stroke tend to have a dual diagnosis of antiphospholipid syndrome and/or the presence of lupus anticoagulant. Additionally, patients with TA who also have anemia and low body mass index (BMI) appear to be at greater risk of cardiovascular disease.
Priscille Couture of the Hopital de la Pitie-Salpetriere in Paris and colleagues described 17 patients with TA and stroke who were treated at a tertiary care center between 2002 and 2016. They published the results of their retrospective, multicenter, case-controlled study online Feb. 1 in the Journal of Neurology. The 17 patients in their study represented 13.5% of the 126 patients diagnosed with TA in their tertiary centers. The investigators sex-matched the 17 individuals to 17 controls with TA who had no neurological signs.1
When the researchers compared patients with TA with patients with TA and stroke, they found that both groups had a similar clinical presentation of TA at diagnosis, as well as comparable cardiovascular risk factors. They also found no significant difference regarding smoking, diabetes mellitus, peripheral artery disease, BMI, coronaropathy or familial history of cardiovascular and cerebrovascular event frequencies. Although the median blood C-reactive protein (CRP) level at TA diagnosis was higher in patients with cerebrovascular events, the difference between the groups was not statistically significant. The investigators note that patients with stroke had more internal carotid artery stenosis than controls.
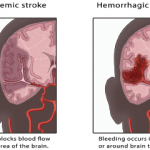
The researchers report that patients in their cohort experienced either ischemic or transient ischemic attack as their first cerebrovascular event. They considered all of these strokes to be linked to TA because of high CRP levels, suggestive imaging results and the exclusion of cardioembolic and artherosclerotic causes. The investigators did not document any hemorrhagic strokes in their cohort. Most of the cerebrovascular events were in the internal carotid artery, particularly in the middle cerebral artery and anterior cerebral artery territories.
In eight patients, stroke occurred a median of 13 years (range: 1–21 years) after the TA diagnosis had been made. In the case of nine patients, stroke was the first symptom of TA. For four patients the stroke occurred after carotid surgery. This finding led the investigators to caution that a risk of stroke associated with performing internal carotid surgery exists in these patients.