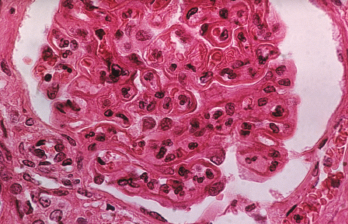
The pattern of lupus glomerular involvement is similar to that in membranous nephropathy, forming wire-loop lesions.
Biophoto Associates / Science Source
The incidence of lupus nephritis in patients with systemic lupus erythematosus (SLE) has decreased over the past 50 years, according to a study from Gabriella Moroni, who works in the Nephrology Unit at Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico in Milano, Italy.1 Typically, renal involvement is part of the disease course for two-thirds of patients, the study authors reported. Renal involvement is a strong predictor of death and end-stage renal disease, but in their cohort, patient and renal survival markedly improved over time.
The authors wanted to examine changes in demographic, clinical and histological features of lupus nephritis, and changes in prognosis. Their retrospective study included 499 patients with lupus nephritis diagnosed between 1970–2016. The inclusion criteria included an SLE diagnosis based on ACR criteria, and biopsy-proven lupus nephritis. The patients were seen at one of four Italian referral centers.
The study’s 46-year follow-up was divided into three time periods of 15 years each: P1=1970–1985, P2=1986–2001 and P3=2002–2016, paralleling major advancements in lupus nephritis treatment.
About 85% of the study patients were women, and almost all were Caucasian; patients were followed for a median of 10.6 years. The number of male patients increased over time, from 6.6% in P1 to 12% in P2 and 19.6% in P3. The researchers noted an increasingly longer lag time between SLE and lupus nephritis diagnosis from 1970–2016 (P<0.0001). Age of lupus nephritis occurrence rose from 28.4 years in P1 to 29 years in P2 and 34.4 in P3 (P<0.001).
Researchers observed a progressive decrease in mean serum creatinine at diagnosis over time (1.8 mg/dL in P1, 1.2 mg/dL in P2 and 1.0 mg/dL in P3), as well as a significant decrease in the frequency of acute nephritic syndrome and rapidly progressive renal insufficiency. Significant growth was found in the prevalence of isolated urinary abnormalities from P1–P3.
Treatment & Outcomes
Among all time periods, more than two-thirds of patients were treated with methylprednisolone pulses as induction therapy. In P1, 29% of patients received induction therapy with corticosteroids alone, compared with 17.9% in P2 and 5.4% in P3. Immunosuppressive drug use grew more common over time, and they were added for maintenance therapy in 30.5%, 65.5% and 89.1% of patients in P1, P2 and P3, respectively. Cyclophosphamide was used by 50% or more of patients in each time period, and there was a decrease in the use of azathioprine as induction therapy from P1–P3; this was counterbalanced by an increase in the use of mycophenolate mofetil.
“Notably, the proportion of patients treated with [immunosuppressive drug] induction therapies progressively decreased over time,” the study says.
Among the 478 patients with outcomes available, 49.6% had complete renal remission in P1, compared with 48.4% in P2 and 58.5% in P3. The incidence of chronic kidney disease and end-stage renal disease lowered over time—it was 7.9% and 24.8% respectively, in P1; 8.5% and 9.1% in P2; and 4.5% and 1.3% in P3 (P<0.0001 for all comparisons). In P1, 20 patients died, compared with nine patients in P2 and eight patients in P3.
The chronic kidney disease-free survival rate at 10 and 20 years was 75% and 66% in P1, respectively; 85.5% and 80.2% in P2; and 91.5% in P3. The end-stage renal disease-free survival at 10 and 20 years was 87% and 80% in P1, respectively; 94% and 90% in P2; and 99% in P3.
Factors independently associated with poor renal outcomes included baseline serum creatine, high activity and chronicity index, arterial hypertension and the absence of maintenance immunosuppressive therapy. “In addition, male gender, older age and high serum creatinine were predictors of death,” the study says. The reason for a larger proportion of male patients over time was not clear to the authors, and they believe this finding should be confirmed in large multicenter studies.
Study limitations include its retrospective nature, no information on patients who achieved remission after induction therapy and the homogenous nature of the study population. However, the authors believe this is the first study that evaluates changes in demographic, clinical and histological features at the time of lupus nephritis presentation.