SAN FRANCISCO—“We haven’t made a lot of progress in ensuring the early diagnosis of spondyloarthritis,” said Walter Maksymowych, MD, FRCP, professor of medicine in the Division of Rheumatology at the University of Alberta and chief medical officer at CaRE (Canadian Research and Education) Arthritis, both in Edmonton.
Speaking at the California Rheumatology Alliance 2016 Medical & Scientific Meeting in May, he offered one reason for this lack of progress: an overreliance on X-ray assessments and insensitive and nonspecific lab tests, along with a failure to take advantage of such technologies as the use of magnetic resonance imaging (MRI) for early diagnosis and classification.
Inflammatory-type back pain is common with lower back pain due to various causes. Spondyloarthritides, a set of chronic diseases of the joints, are diagnosed based on lab tests, imaging tests and inflammatory symptoms. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat pain and inflammation, but when these don’t provide relief, doctors often prescribe disease-modifying anti-rheumatic drugs (DMARDs) similar to those used in rheumatoid arthritis, but these are not effective.
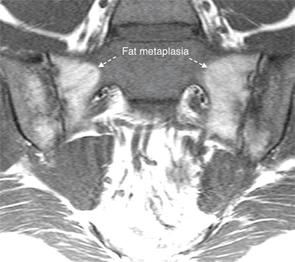
“You can measure inflammatory markers, such as C-reactive protein, but they lack sensitivity and specificity,” Dr. Maksymowych explained. Diagnosis of spondyloarthritis by X-ray for a complex structure, such as the sacroiliac joint, doesn’t identify early changes and is unreliable until more advanced stages of the disease—at a point of functional impairment. “There’s a great deal of subjective interpretation required. It’s not surprising that rheumatologists have trouble with it,” he said.
“The shame is that there are effective treatments, but we don’t get to them soon enough because we aren’t using MRI.” There is good evidence that the sooner you treat, the more impressive the results, with the possibility for remission of symptoms. Earlier diagnosis might also mean earlier access to biologic therapies. “We might be able to slow progression of disease. Will early treatment stop spine damage? We can’t begin to explore the possibilities if we don’t make earlier diagnoses.”

Dr. Maksymowych
For Dr. Maksymowych, the MRI is the imaging modality of choice for early diagnosis of sacroiliac lesions in inflammatory back pain in settings where crucial treatment decisions are made. But interpreting MRIs for this purpose requires a level of comfort with the DICOM (Digital Imaging and Communications in Medicine) image standard for handling, storing and transmitting medical images. DICOM is the international standard for medical imaging and requires special software for the images to be seen.
