A few months later, the patient developed a small bowel obstruction as a result of adhesions. His hospitalization was complicated by the development of pleural effusion requiring thoracentesis. He also experienced a 30 lb. weight loss and severe deconditioning, requiring total parenteral nutrition for bowel rest. Additionally, he developed a new supraventricular tachycardia.
Once again the search for answers started.

Lesson Learned from a 2nd Patient
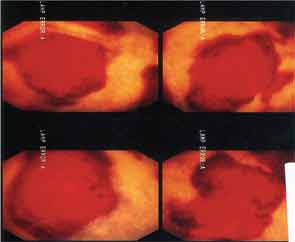
With the unique nature of MAP skin lesions, we were able to identify similar lesions on another patient previously diagnosed with an overlap syndrome with features of systemic lupus erythematous and systemic sclerosis. The skin lesions were biopsied and were reported as MAP-like lesions. Subsequently, the patient was started on subcutaneous treprostinil for treatment of her severe pulmonary hypertension. Interestingly, within three months of initiating therapy with treprostinil, her MAP-like skin lesions showed marked involution (see Figure 4).
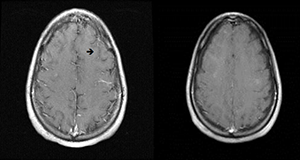
Based on these findings, in December 2010, we were able to obtain treprostinil on a compassionate-use basis for our 17-year-old male patient. Slowly, he improved and has been maintained on a regimen of treprostinil, eculizumab and aspirin.
Repeat MRI of the brain showed complete resolution of brain lesions (see Figure 5). He continues to develop some skin lesions, but they involute more quickly and remain smaller in size compared with presentation prior to treatment.
A 3rd Patient
Our 17-year-old patient’s sister was found to have biopsy-proven MAP skin lesions. She underwent exploratory laparoscopy to evaluate complaints of abdominal pain, and no serosal lesions were seen. The pain spontaneously resolved. It appears that she has cutaneous disease only.
What Is Malignant Atrophic Papulosis?
MAP is an uncommon thrombo-occlusive vasculopathy with characteristic skin lesions.1 Similar lesions can affect internal organs, such as the GI tract, central nervous system, pericardium and bladder.2 Thrombotic complications with characteristic infarcted zones can be seen on histopathology.3,4 Cutaneous-only involvement has been described. Conversely, previously reported systemic disease has been fatal.