Angioimmunoblastic T cell lymphoma (AITL) is an aggressive, peripheral T cell, non-Hodgkin’s lymphoma with an incidence of 0.05 cases per 100,000 person-years in the U.S., and it typically manifests in adults older than 60 years.1,2
AITL was previously known as angioimmunoblastic lymphadenopathy with dysproteinemia, immunoblastic lymphadenopathy or lymphogranulomatosis X, due to the hypothesis that the disease was an immune dysregulation of both B and T cells.1,3 Subsequent advancements in genomic studies uncovered its true pathogenesis as a primary T cell malignancy. AITL has a multitude of clinical presentations with notable systemic B symptoms: splenomegaly, hepatomegaly, polyarthritis and generalized lymphadenopathy.
In this article, we present the case of a patient diagnosed with AITL and referred to a rheumatologist for the management of rheumatoid factor-positive polyarthritis, suspicious for rheumatoid arthritis (RA).
The Case
A 71-year-old white man was referred to a community hospital rheumatology clinic in September 2017 for evaluation of a month-long history of generalized arthralgias. A month earlier, the patient had been evaluated by his primary care provider in a routine checkup. A pneumococcal vaccination was administered, and within 24 hours the patient’s arthralgias began. He also reported worsening malaise, fatigue, nausea and subjective fevers that had occurred over the preceding several weeks. Concerned for infection, his doctor hospitalized the patient briefly. After tests for infection proved negative, the patient was started on prednisone at 20 mg daily, his symptoms improved substantially, and he was discharged home.
During the patient’s initial workup in the rheumatology clinic, he was tested for rheumatoid factor, which was positive at 47 IU/mL (normal <15). Anti-cyclic citrullinated peptide (anti-CCP), IgG, erythrocyte sedimentation rate, C-reactive protein and hepatitis B and C screening tests were normal or negative.
Radiographs of the hands taken in September 2017 demonstrated no erosions. His prednisone dosage was decreased, but the decrease to 15 mg daily led to a substantial worsening of his symptoms. Methotrexate 15 mg once a week was then added to his prednisone (held at 20 mg daily), but again when prednisone was tapered, his symptoms quickly returned.
Computed tomography (CT) imaging of his chest, abdomen and pelvis in late 2017, pursued out of concern he had an illness other than RA (see Figure 1A), was unremarkable.
Sulfasalazine and hydroxychloroquine were added, but his symptoms persisted. Ultimately, tumor necrosis factor (TNF) inhibitors were added, but tapering of other medications, specifically prednisone, led to the return of symptoms.
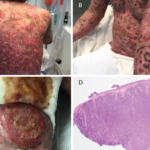
In May 2018, the patient was evaluated in the emergency department of the same hospital for possible diverticulitis. CT scans demonstrated bulky retroperitoneal and abdominal lymphadenopathy (see Figure 1B, below). He was hospitalized, and a biopsy of a retroperitoneal lymph node revealed AITL. Bone marrow biopsy showed similar involvement. Histologic findings demonstrated a marked proliferation of small- to medium-sized lymphocytes with clear cytoplasm, in addition to increased arborizing high endothelial venules (see Figures 2A–2B8).