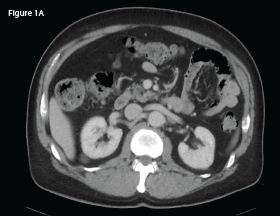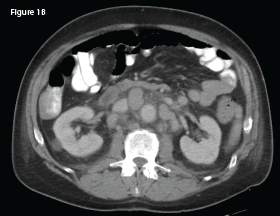
This CT of the abdomen from May 2018 demonstrates interval development of intra-abdominal lymphadenopathy (indicated by the white arrow).
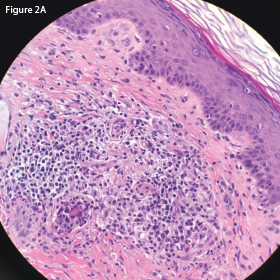
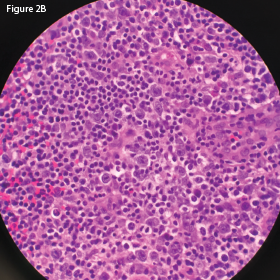
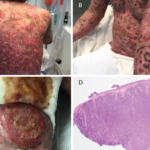
Immunohistochemistry staining demonstrated a diffuse predominance of CD3 positive T cells (see Figure 2C, p. 28). Flow cytometry was notable for an expanded population of CD3-positive T cells.
The patient was evaluated by oncology and treated with CHOEP (cyclophosphamide, doxorubicin, etoposide, vincristine and prednisone). Despite treatment, he experienced a rapid decline in his health, with cutaneous metastases developing in late 2018 and recurrent hypercalcemia in early to mid-2019. He succumbed to his AITL in mid-2019.