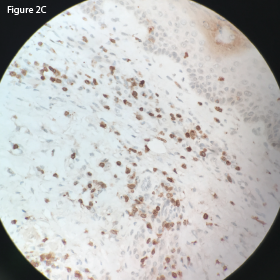
This CD3 stain at 40x magnification of the retroperitoneal lymph node demonstrates
diffuse uptake.
A case report in 1982 by Meyers et al. discussed a patient who presented with generalized arthralgias and failure to respond to conventional therapy for RA who was subsequently diagnosed with AITL.5
Another case report in 1986 by Bignon et al. reported the development of AITL in a patient with sicca symptoms.8 AITL has been reported to arise from extra-nodal lymphoid tissue, and in the case reported by Bignon et al., lymphoproliferation was observed involving the lip of the patient with the immunohistological comparison similar to the primary site of the kidney.9-11