 Inebilizumab reduces the risk of immunoglobulin G4-related disease (IgG4-RD) flares and increases the likelihood of flare-free, complete remission at one year, a recent study shows.1 The randomized, doubleblind, placebo-controlled MITIGATE trial showed that inebilizumab reduced the risk of IgG4-RD symptoms by 87%, compared with placebo.
Inebilizumab reduces the risk of immunoglobulin G4-related disease (IgG4-RD) flares and increases the likelihood of flare-free, complete remission at one year, a recent study shows.1 The randomized, doubleblind, placebo-controlled MITIGATE trial showed that inebilizumab reduced the risk of IgG4-RD symptoms by 87%, compared with placebo.
About IgG4-RD
IgG4-RD is chronic, rare condition that has, so far, been estimated to affect fewer than 200,000 people in the U.S. The systemic, autoimmune inflammatory disease leads to lesions rich in CD19+ B cells. These cells are thought to directly drive inflammation, and scarring and thickening of tissue directly through cytokines, proteins that affect the immune system. The cells may also indirectly activate pathogenic T cells.
Patients with IgG4-RD suffer from the build-up of immune cells, which produce the IgG4 antibody in certain organs. Commonly affected organs include the pancreas, bile ducts, salivary glands, abdominal tissue, eyes and lungs. Symptoms vary, depending on the affected organ. For example, the disease commonly affects the pancreas, causing pancreatitis and diabetes. When the disease affects eye tissues, patients may suffer double vision. Often multiple organs are affected. Many patients undergo a long diagnostic journey and are initially misdiagnosed, some even undergoing unnecessary surgery.
Currently, there is no approved drug for IgG4-RD. The usual, standard treatment for IgG4-RD is prednisone, which reduces disease flares but is problematic.
“Prednisone is toxic for patients, who tend to be middle aged or elderly at the time they’re diagnosed. This is compounded by the fact that IgG4-RD patients often have pancreatic problems—either endocrine or exocrine insufficiency or both—because of the tendency of the disease to target the pancreas,” says the study’s first author, John H. Stone, MD, MPH, a professor of medicine at Harvard Medical School, Boston, and a rheumatologist in the Division of Rheumatology, Allergy, and Immunology at Massachusetts General Hospital (MGH), Boston. “That standard of care [may] be replaced by a medication that will allow patients to be on essentially no steroids after a very short period of time.”
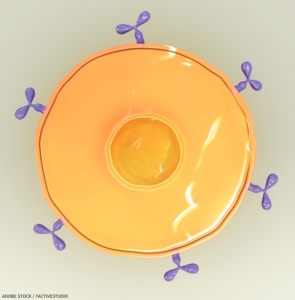
Inebilizumab, manufactured by Amgen, the study’s sponsor, depletes CD19-expressing B cells. The biologic is a lab-created protein designed to mimic a naturally occurring antibody to target the CD-19 antigen.
The Study
The phase 3 MITIGATE trial examined the efficacy and safety of inebilizumab in reducing flare risk for adults with IgG4-RD. The researchers studied 135 participants who were randomized one to one to receive 300 mg of intravenous inebilizumab or placebo on days 1 and 15, and at week 26 after premedication. The participants were followed for a 52-week randomized control period.
The primary end point was time to first treated adjudicated IgG4-RD flare. Secondary end points were annualized flare rate; flare-free, treatment-free remission; treatment-free complete remission; and flare-free, corticosteroidfree complete remission.
In addition to finding that inebilizumab reduced the risk of symptoms by 87%, compared with placebo, for IgG4-RD, researchers found that 40 patients (59.7%) in the placebo group experienced one or more flares, while only seven (10%) in the inebilizumab group experienced at least one flare.
The annualized flare rate was 0.10 for 68 patients on inebilizumab vs. 0.17 for the 67 patients who received placebo. More participants in the inebilizumab group (39) than in the placebo group (15) had flare-free, treatment-free complete remission. Forty inebilizumab patients had glucocorticoid-free complete remission vs. 15 placebo patients.
Participants who received inebilizumab required lower cumulative glucocorticoid exposure to induce remission and maintain disease control during the treatment period than participants who received placebo.
The number of participants who had at least one adverse event during the treatment period was similar in the two groups—66 participants in the inebilizumab group, or 97%, and 66 participants in the placebo group, or 98%.
However, participants on inebilizumab had more serious adverse events of grade 3 or higher that required a medical intervention or significantly disrupted daily life. Grade 3 adverse events occurred in 12 participants, or 18%, in the inebilizumab group and eight participants, or 12%, in the placebo group. Serious adverse events occurred in 12 inebilizumab participants (18%) and six placebo participants (9%), respectively. No single participant experienced more than one serious adverse event.
Adverse events that occurred in more than 10% of participants in the inebilizumab group included COVID-19 among 16, or 24%, of participants. Other adverse events among the inebilizumab group were lymphopenia in 11 participants, or 16%, and urinary tract infection in eight participants, or 12%. Lymphopenia was the most common adverse event of special interest observed in both the inebilizumab and placebo groups. Other infections reported by patients who received inebilizumab were urinary tract infection, nasopharyngitis, upper respiratory tract infection and influenza.
The researchers noted their trial’s limitations. They include its modest size and the low number of participants with previous IgG4-RD treatment. However, the researchers write that they noted no reason to suspect that previous treatment affected trial outcomes. Also, the study population’s median disease duration was relatively short, 3.6 years, among 54% of the participants with recurrent disease at baseline. Because study criteria included history of involvement of at least two organs, some patients with IgG4-RD in just one organ were potentially excluded, the researchers add.
Considerations & Implications
The trial was the culmination of 15 years of work after Dr. Stone first used a B cell-depleting agent and was “astonished by the perceived efficacy of B cell depletion” in four IgG4-RD patients.
The results of the current trial—conducted at 80 sites in 22 countries—confirm the efficacy of B cell depletion. “The overwhelming efficacy of B cell depletion underscore the reason that it’s important to identify the disease, because IgG4-RD participants with it respond so well to (inebilizumab) therapy,” Dr. Stone says.
First recognized as a unique condition in 2003, IgG4-RD has thus far been considered a rare disease. However, it is difficult to differentiate IgG4-RD from conditions that rheumatologists see often, such as anti-neutrophil cytoplasmic autoantibody (ANCA) associated vasculitis, Sjögren’s disease, systemic lupus erythematosus, sarcoidosis and aortitis, Dr. Stone points out.
“Rheumatologists are highly likely to see many patients with this disease over the course of their careers, because this is not a vanishingly rare condition at all,” he maintains. “The epidemiology so far suggests that IgG4-related disease may be as common as, or even more common than, some of those. If rheumatologists feel like they’re not seeing it in their practice, my strong suspicion is that they’re missing the diagnosis and may be considering it to be something else.”
Unlike most autoimmune diseases, IgG4-RD affects more men than women. An additional consideration for managing the disease is that often affects the sexes differently. Other recent research by Dr. Stone shows that 50% of men are affected in the pancreas vs. only 26% of women. Renal involvement affects 39% of men vs. 18% of women. The disease is likely to be more severe in men.2
Inebilizumab is currently marketed by Amgen as UPLIZNA for treatment of a rare autoimmune disease of the central nervous system, neuromyelitis optica spectrum disorder.
Dr. Stone is hopeful that the overwhelmingly positive results from his phase 3 trial will lead to U.S. Food & Drug Administration (FDA) approval of inebilizumab to treat IgG4-RD, and then approval by regulatory agencies in other countries. The FDA is currently reviewing a submission for inebilizumab to treat IgG4-RD.
Deborah Levenson is a writer and editor based in College Park, Md.
References
- Stone JH, Khosroshahi A, Zhang W, et al. for the MITIGATE Trial Investigators. Inebilizumab for treatment of IgG4-related disease. N Engl J Med. 2024 Nov 14. Online ahead of print.
- Jha I, McMahon GA, Perugino CA, et al. Sex as a predictor of clinical phenotype and determinant of immune response in IgG4-related disease: A retrospective study of patients fulfilling the American College of Rheumatology–European League Against Rheumatism classification criteria. Lancet Rheumatol. 2024 Jul;6(7):e460-e468.
Disclosure
Dr. Stone has received consulting fees from Amgen related to IgG4-RD, glucocorticoid toxicity and systemic vasculitis.