Methods: We randomly assigned 283 patients who had had severe sciatica for six to 12 weeks to early surgery or to prolonged conservative treatment with surgery if needed. The primary outcomes were the score on the Roland Disability Questionnaire, the score on the visual-analogue scale for leg pain, and the patient’s report of perceived recovery during the first year after randomization. Repeated-measures analysis according to the intention-to-treat principle was used to estimate the outcome curves for both groups.
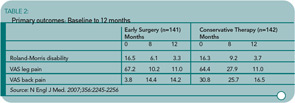
Results: Of 141 patients assigned to undergo early surgery, 125 (89%) underwent microdiscectomy after a mean of 2.2 weeks. Of 142 patients designated for conservative treatment, 55 (39%) were treated surgically after a mean of 18.7 weeks. There was no significant overall difference in disability scores during the first year (p=0.13). Relief of leg pain was faster for patients assigned to early surgery (p<0.001). Patients assigned to early surgery also reported a faster rate of perceived recovery (hazard ratio 1.97; 95% confidence interval 1.72 to 2.22; p<0.001). In both groups, however, the probability of perceived recovery after one year of follow-up was 95%.
Conclusions:
The one-year outcomes were similar for patients assigned to early surgery and those assigned to conservative treatment with eventual surgery if needed, but the rates of pain relief and of perceived recovery were faster for those assigned to early surgery.
Commentary
The patient with leg pain associated with a herniated intervertebral disc faces a number of treatment options. A herniated disc may heal spontaneously over a time period measured in months. Medical therapy including nonsteroidal anti-inflammatory drugs, analgesics, oral and/or injectable corticosteroids, and physical therapy can ease pain and decrease inflammation of damaged tissues during this time of disc resorption. Surgical intervention removes the offending piece of herniated nucleus pulposus with almost immediate resolution of leg pain. When patients are offered all of these options, the question frequently asked by those considering surgery is, What is the timeframe for a good outcome from an operation? The commonly quoted dictum is that surgery needs to be undertaken within 12 weeks of the onset of sciatica to have the best result.1 Peul and co-workers would disagree and state that the window of opportunity for a successful surgical outcome is six months or longer.
In the Peul study, one cohort of patients who had not improved between six to 12 weeks after a disc herniation underwent surgery within two weeks of evaluation (early surgery group). Patients who were assigned to conservative therapy could opt for surgery if they had no improvement. The average time for the 40% of medically treated patients who went on to surgery was 4.5 months. The one-year outcomes of the entire surgical and conservative treatment groups were similar. The difference was the earlier resolution of disability and pain in the surgical cohort. (See Table 2)