Given the evolution of her skin lesions despite steroids, the differential diagnosis included infectious vs. autoimmune conditions, such as bullous lupus, which can be resistant to steroid treatment. Dapsone was initiated while awaiting the result of skin biopsies.
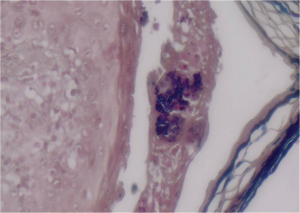
Figure 3: (Gram stain 60x) Gram-positive cocci aggregated in colonies within the vesicle.
Microbiological examination of serous fluid from the cutaneous blisters grew methicillin-resistant Staphylococcus aureus (MRSA) (see Figure 3). Histopathology from the skin biopsies revealed the presence of interface vacuolar dermatitis (see Figure 4) with cytoid bodies, as can be seen in autoimmune conditions and superficial and mid epidermal acantholysis (see Figures 5 and 6), for which the differential diagnoses were pemphigus foliaceous and Staphylococcal scalded skin syndrome. Direct immunofluorescence showed a continuous granular reaction for both IgG and IgM at the dermo-epidermal junction (positive lupus band). ELISA was negative for Desmoglein 1 and 3. The final pathology result suggested a combined presence of a flare of lupus erythematosus with a Staphylococcal scalded skin syndrome.
The patient was receiving intravenous and topical antibiotics including coverage for MRSA, but given the lack of an immediate response, she went on to receive intravenous immunoglobulins, which led to a significant improvement of her rash (see Figure 7).
Discussion
Acute-onset bullous lesions in any patient need to be addressed with due caution, with considerable emphasis on ruling out life-threatening dermatological emergencies, such as Stevens Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN), and consideration of an infectious etiology (especially in patients on immunosuppressive therapy) or other autoimmune conditions, such as pemphigus. Given the extent of overlapping clinical symptoms of bullous lesions, a skin biopsy is critical because a careful histopathological examination and immunohistochemical staining are essential to confirm the diagnosis.
Lupus can present with a wide variety of cutaneous manifestations, ranging from papules and plaques to vesiculo-bullous lesions.1,2 Acute cutaneous lupus can present as an erythematous malar rash typically sparing the nasolabial fold and can evolve into vesiculo-bullous lesions.2,3
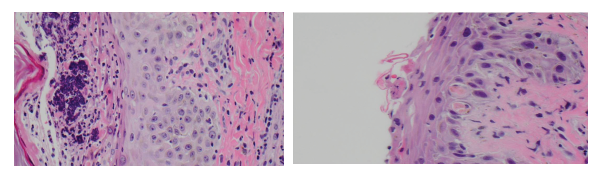
(left) Figure 4: (H&E 60x) Interface vacuolar dermatitis and a superficial vesicle with neutrophils and bacterial colonies.
(right) Figure 5: (H&E 60x) Interface vacuolar dermatitis with two cytoid bodies; note the superficial acantholysis of the epidermal cells.
Subacute cutaneous lupus involves the upper neck, chest, back and the extensor surfaces of arms and forearms, sparing the scalp and knuckles, and manifests as papules or annular plaques. This condition is rarely associated with systemic manifestations. Chronic cutaneous lupus or discoid lupus manifests as coin-shaped lesions with a hypopigmented center.2,3



