Andrey_Popov/shutterstock.com
We report a case of a 27-year-old woman who was initially diagnosed with systemic lupus erythematosus (SLE), had features of scleroderma and was subsequently found to have lymph node biopsy consistent with multicentric Castleman disease (MCD). She also had serologic evidence of acute Epstein-Barr virus (EBV) infection (vs. reactivation of EBV). The occurrence of MCD in association with SLE and scleroderma is rare, and the relationship between these diseases and EBV remain areas of ongoing research. We report this case to increase awareness of this potential diagnostic and therapeutic dilemma.
Case
The patient is a 27-year-old African Caribbean woman who initially presented with malaise, dry cough, weight loss of 25 lbs. over four months, diffuse arthralgia, myalgia, hair loss, diaphoresis, numbness of extremities, bilateral ankle swelling, cold intolerance and Raynaud’s phenomenon. She was febrile, temperature 101.8º F, blood pressure of 102/57 mmHg, pulse of 111 bpm and respiratory rate of 24 breaths per minute. On physical exam she was cachectic, with tightness around the mouth, telangiectasia over the nasal bridge, digital ulcer on the left third digit, soft abdomen with hepatosplenomegaly, pitting edema of the lower extremities, bilateral axillary and femoral lymphadenopathy.
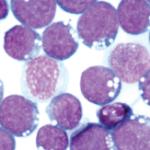
Labs were significant for hemoglobin (Hb) of 5.6 g/dL (normal range: 12–16 g/dL), a reticulocyte count of 3.11% (normal range: 0.5–2.9%), LDH 664 U/L (normal range: 135–214 U/L), haptoglobin of 3 mg/dL (normal range: 30–200 mg/dL), ferritin 589.7 ng/mL (normal range: 10–291 ng/mL), direct Coombs test positive for nonspecific cold agglutinin, an unremarkable peripheral blood smear and an ESR of 129 mm/hr (normal range: 0–20 mm/hr). She had an albumin of 2.6 g/dL (normal range: 2.8–5.7 g/dL) and 2+ proteinuria on dipstick. RF, ANA and c-ANCA were negative, but p-ANCA was positive. C3 was 45 mg/dL (normal range: 86–184 mg/dL) and C4 was 7 mg/dL (normal range: 20–58 mg/dL). HIV, human T cell lymphoma virus 1 (HTLV 1), hepatitis B and C screening, RPR, PPD and blood cultures were negative.
A non-contrast CT scan of the chest revealed bilateral axillary lymphadenopathy measuring up to 1.5 cm, trace bilateral pleural effusions and small pericardial effusion, but no consolidation. A CT scan of the abdomen with contrast revealed bulky retroperitoneal and pelvic lymphadenopathy with bulky external iliac nodes, the largest of which was 4.4 x 1.7 cm, ascites, hepatosplenomegaly, periportal edema, perihepatic ascites and pericholecystic fluid. 2D echo revealed an ejection fraction of 55–60%, mild tricuspid regurgitation, estimated pulmonary arterial pressure of 40 mmHg and a small to moderate pericardial effusion.