Depending on stage, severity and rate of progression of disease, systemic corticosteroids are commonly used to treat pulmonary sarcoidosis. However, a review of the literature suggests they have limited usefulness in advanced stage IV pulmonary sarcoidosis. Once sarcoidosis has advanced to this degree, steroid use may unnecessarily expose a patient to life-threatening complications, as demonstrated in this report.
Case Presentation
A 41-year-old man presented to the emergency department with massive hemoptysis that resulted in a cardiac arrest. With emergent resuscitation, return of spontaneous circulation was achieved, and the patient was intubated for hypoxic respiratory failure, requiring mechanical ventilation. His medical history was significant for a 10-year history of pulmonary sarcoidosis and steroid-induced diabetes. His medication regimen included prednisone, 20 mg twice daily, which he had been taking for the preceding four months.
A chest CT (see figures below and on p. 24) demonstrated advanced, Stage IV pulmonary sarcoidosis with significant architectural distortion related to multiple mycetomas visualized in the left upper lobe, right middle lobe and right upper lobe, and markedly distorted bronchiectatic airways connecting to the dominant mycetomas. Pulmonary angiography localized bleeding from both bronchial arteries, as well as a branch of the right bronchial artery, which was supplying the right upper lobe. Interventional radiology performed successful particle embolization of the culprit arteries.
Pulmonary hypertension is commonly seen in Stage IV sarcoidosis, & steroids have not been shown to result in a significant hemodynamic response in this subset of patients. Thus, the role of steroids in advanced stage IV disease is limited.
Laboratory studies were significant for a positive Platelia (ELISA for Aspergillus) of 5.27 (index ≥0.5 is positive) and Fungitell assay greater than 500 pg/mL (glucan values ≥80 pg/mL are positive), confirming aspergillosis. Voriconazole therapy was initiated, and the patient was discharged home with a steroid taper schedule. After further evaluation, he underwent lung transplantation two months later.
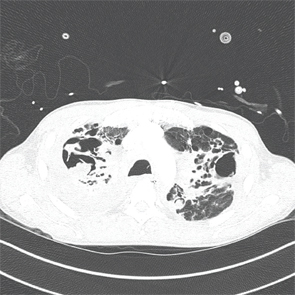
An axial CT view demonstrating a large mycetoma in the right upper lobe and a left upper lobe cavitating lung lesion.
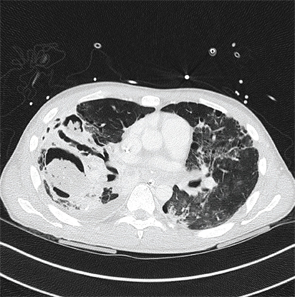
An axial CT view demonstrating a mycetoma in the right lower lobe.
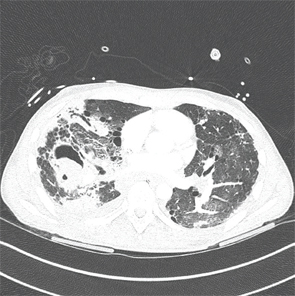
An axial CT view demonstrating a mycetoma in the right middle lobe.
Discussion
Asymptomatic pulmonary sarcoidosis, regardless of stage, does not require the initiation of steroid therapy, but rather should be monitored for clinical progression. Steroids should be considered in patients with significant symptoms (e.g., cough, dyspnea, hemoptysis), worsening radiographic findings and worsening pulmonary function tests.1
When treating patients with steroids, the recommended starting dose is 20–40 mg prednisone daily.2 If there is a response over the next one to three months, the dose should be tapered to 5–15 mg daily and then continued for nine to 12 months.2 The presence of irreversible Stage IV fibrotic disease is a potential reason that a patient may not respond to steroids, because these patients may not have active inflammation for which steroids can be effective.3
It should be noted that this patient had highly advanced Stage IV disease and had been treated with high-dose prednisone for over three months at the time of his massive hemoptysis. In addition, pulmonary hypertension is commonly seen in Stage IV sarcoidosis, and steroids have not been shown to result in a significant hemodynamic response in this subset of patients. Thus, the role of steroids in advanced Stage IV disease is limited.4
Given the potential adverse effects of their chronic use, frequent clinical reassessments should be made to evaluate the continued need for and appropriate dosage of steroids in pulmonary sarcoidosis. In addition to the well-known effects on bone health and the endocrine system, steroids increase the risks of opportunistic infections that can be life threatening.
When patients with pulmonary sarcoidosis who are being treated with steroids develop clinical changes, such as hemoptysis, a low threshold for imaging is required. The estimated incidence of chronic cavitary aspergillosis in sarcoidosis is 2%, and hemoptysis is an important complication of this infection, which can present with a wide range of signs and symptoms.5
Hemoptysis is thought to arise from local vascular invasion by the Aspergillus organism, and it can result in life-threatening bleeding, as seen in this patient. Itraconazole, voriconazole and even intracavitary amphotericin B and voriconazole have been used to treat aspergillomas, but the treatment of these infections in sarcoidosis is not well established.4
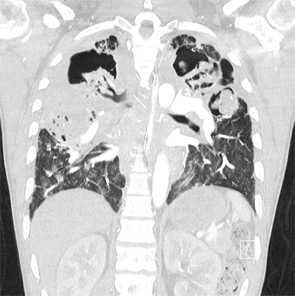
A coronal CT view demonstrating right and left upper lobe mycetomas.
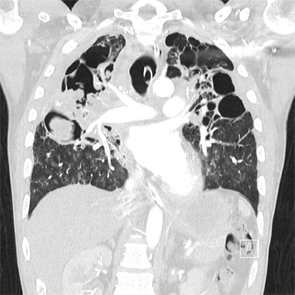
A coronal CT view demonstrating right upper and middle lobe mycetomas.
Conclusion
The potential role and appropriate dosage of corticosteroids should be carefully evaluated in patients with pulmonary sarcoidosis. These patients should be monitored for changes in symptoms, including worsening cough, hemoptysis and dyspnea, because these may imply worsening sarcoidosis, but they should also be evaluated thoroughly to rule out infection, malignancy or worsening pulmonary hypertension. Steroids carry significant and potentially life-threatening risks and are not warranted in all patients with this disease.
 Josna Haritha, MD, MPH, completed medical school at University of Alabama at Birmingham in 2013 and finished an internal medicine residency at Virginia Commonwealth University (VCU) in 2016. She now works as a hospitalist at the McGuire VA Hospital.
Josna Haritha, MD, MPH, completed medical school at University of Alabama at Birmingham in 2013 and finished an internal medicine residency at Virginia Commonwealth University (VCU) in 2016. She now works as a hospitalist at the McGuire VA Hospital.

Derick N. Jenkins, MD, completed medical school at Dartmouth in 2011 and finished an internal medicine residency at VCU in 2016. He now serves as a chief medical resident.
 Manpreet S. Malik, MBBS, is an assistant professor in the Department of Internal Medicine at Virginia Commonwealth University School of Medicine in Richmond, Va. He completed his residency in internal medicine at UPMC, Pittsburgh and joined VCU Health in 2013 as an academic hospitalist. His areas of expertise are ultrasound-guided bedside procedures, case-based learning, faculty development and technology, and mobile apps in medicine.
Manpreet S. Malik, MBBS, is an assistant professor in the Department of Internal Medicine at Virginia Commonwealth University School of Medicine in Richmond, Va. He completed his residency in internal medicine at UPMC, Pittsburgh and joined VCU Health in 2013 as an academic hospitalist. His areas of expertise are ultrasound-guided bedside procedures, case-based learning, faculty development and technology, and mobile apps in medicine.
References
- Bradley B, Branley HM, Egan JJ, et al. Interstitial lung disease guideline: The British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax. 2008 Sep;63(Suppl 5):v1–v58.
- Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Eng J Med. 2007 Nov 22;357(21):2153–2165.
- Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med. 1999 Aug;160(2):736–755.
- Shlobin OA, Nathan SD. Management of end-stage sarcoidosis: Pulmonary hypertension and lung transplantation. Eur Respir J. 2012 Jun;39(6):1520–1533.
- Pena TA, Soubani AO, Samavati L. Aspergillus lung disease in patients with sarcoidosis: A case series and review of the literature. Lung. 2011 Apr;189(2):167–172.


