Study Impact
The paper attracted much interest and served as the focus of a plenary session at that year’s ACR/ARHP Annual Scientific Meeting. Due to its influence, physicians became much more likely to prescribe hydroxychloroquine over the long term. Sales of the drug, still under patent then, went up markedly after the paper’s release.
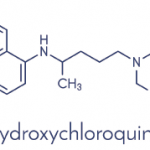
Today, hydroxychloroquine is a staple treatment of lupus. In the absence of rare contraindications, most experts recommend lifelong treatment with hydroxychloroquine for all lupus patients, regardless of disease severity or additional therapies.
“The study demonstrated that hydroxychloroquine wasn’t just for active lupus, but had a major preventive role,” Dr. Petri says.
In addition to lupus, hydroxychloroquine is less frequently used to treat RA and certain other inflammatory rheumatologic diseases. The drug is also under consideration for new applications, such as heart disease, diabetes mellitus and certain cancers.8
Since the initial study by the Canadian Hydroxychloroquine Study Group, researchers in other follow-up studies have confirmed the important role of hydroxychloroquine in preventing lupus disease flares. Scientists have also learned much about the drug’s multiple beneficial effects. Over the years, it has become evident that hydroxychloroquine does more than suppress mild disease, as was initially believed.
Explains Dr. Petri, “I’ve spent the past 34 years trying to build on what the Canadians showed back in 1991. We know now [hydroxychloroquine] helps improve survival; it reduces cardiovascular risk factors, thrombosis, renal damage, central nervous system lupus and more.”
A population-based, case-controlled study from 2019 demonstrated that mortality risk increased almost fourfold in people who had to stop taking their hydroxychloroquine.9 It is the only drug that has been demonstrated to improve the survival of lupus patients. Hydroxychloroquine also appears to be a safe and effective drug in pregnant patients, reducing flares during this time and decreasing the risk of cardiac neonatal lupus.6
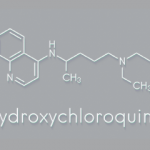
Continued Safety Concerns for Hydroxychloroquine
Although the potential impact of hydroxychloroquine is undeniable, its safety is again being questioned. For reasons that are unclear, the incidence of retinopathy appears to have been increasing in recent years. Dr. Petri notes that research has demonstrated that retinopathy from hydroxychloroquine is more common than previously thought. This is a major concern, because late retinopathy is not reversible, and no currently available therapies can treat it.8
Dr. Petri et al. recently published an article demonstrating that about 11% of lupus patients taking hydroxychloroquine will have to stop it after 16 years due to signs of early retinopathy.10 Dr. Petri explains this may be due to the greater sensitivity of newer ophthalmology screening tests for retinopathy, such as optical coherence tomography (OCT), which may be picking up milder retinopathy at a much earlier stage than was possible in the past.
“We are facing the fact that hydroxychloroquine is not going to be allowed in every single patient for their lifetime of lupus,” she says. “I’m always annoyed when I get a note from an ophthalmologist who tells me to start a substitute for hydroxychloroquine due to retinopathy. We do not have a substitute for it; we have nothing to replace it.”
She hopes this will serve as an impetus for the research community to find better or additional lupus therapies.
In 2016, the American Academy of Ophthalmology published guidelines for hydroxychloroquine patient monitoring, recommending OCT at baseline, five years thereafter and then every year following for patients without major risk factors for retinopathy.8
Questions also remain about optimal dosing of the drug. Higher doses have been associated with a greater risk of retinopathy. In terms of toxicity, recent guidelines from the American Academy of Ophthalmology recommend lowering the dosage from 6.5 mg/kg patient weight to less than 5.0 mg/kg.8
Dr. Petri responds, “The concern has been, if you reduce the dose, we’re going to reduce the efficacy.” At the 2019 ACR/ARP Annual Meeting, Dr. Petri presented data demonstrating that lowered blood levels of hydroxychloroquine did, in fact, increase the risk of thrombosis in lupus patients.11
Hydroxychloroquine blood levels may provide a way to find optimal efficacy with a lower risk of retinopathy. Dr. Petri explains, “Blood levels reflect how much the patient has taken over the past month, very similar to a hemoglobin A1c in diabetes; it’s really reflective of their adherence.” She believes these blood levels can help identify people who are taking more hydroxychloroquine than needed—people who could safely have their dose lowered.
Hydroxychloroquine blood levels are becoming more universally available. Dr. Petri explains that Exagen provides a commercial source, and labs like Quest Diagnostics also offer them. “Some other labs,” she notes, “have offered plasma levels, which aren’t as accurate. Hydroxychloroquine binds to red cells, so plasma grossly underestimates the actual exposure. This is a field in flux—using therapeutic blood monitoring to guide dosing of hydroxychloroquine, so that we do not give too little or too much.”