 How to Manage Organ Manifestations of Sarcoidosis & Help Patients
How to Manage Organ Manifestations of Sarcoidosis & Help Patients
EULAR 2024 (VIENNA)—Sarcoidosis: It’s a multi-system inflammatory disease that triggers many referrals to rheumatology—and perhaps just as many groans from the rheumatologists who receive those referrals. But why? After all, who better to manage a multi-system inflammatory disease than a rheumatologist?1
At EULAR 2024, Arthur M.F. Yee, MD, PhD, director, Hospital for Special Surgery Sarcoidosis Collaborative, HSS/Weill Cornell Medicine, New York, championed and encouraged the rheumatologist’s involvement in the care of patients with sarcoidosis. It was a great session, and quite frankly, a peptalk that many of us—myself included—needed to hear.
Sarcoidosis Needs a Rheumatologist
Dr. Yee
Dr. Yee opened his session with a call to action.
“When I was first asked to speak, the title I was given was ‘Sarcoidosis: Joint, Bone and Muscles,’ and I badgered the organizers to let me change it,” he said. “I changed it to ‘Sarcoidosis: (Not Just) Bone, Joint and Muscles’ because I think the role of rheumatologists has been understated. We need to take a stronger role in taking care of these patients as individuals and as a community.”
Dr. Yee shared two timelines depicting when certain medications, including prednisone, chloroquine, methotrexate, infliximab and tofacitinib, should be introduced for the treatment of rheumatoid arthritis (RA) and sarcoidosis (see Figure 1). “As you can see, in every case, the use of medications for RA precedes those for sarcoidosis by many years,” he said. “So I would wager a guess that many of the medications we are talking about outside right now in poster form may have applicability to sarcoidosis going forward.”
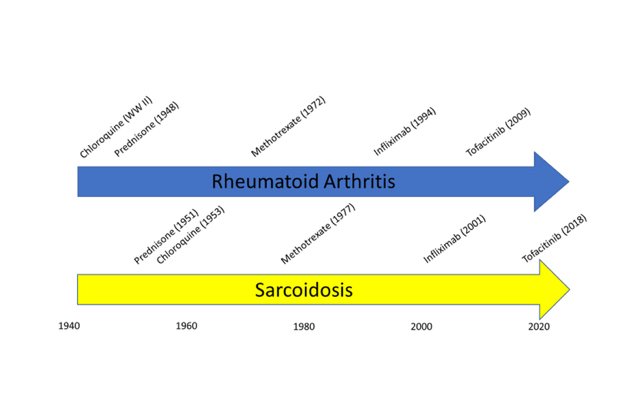
Figure 1: Timeline comparing when medications were introduced for RA vs. sarcoid.
Why aren’t rheumatologists more interested in sarcoidosis? The condition is similar to so many diseases we don’t hesitate to manage, such as systemic lupus erythematosus. Like lupus, sarcoidosis is a multi-system disease of immunologic dysregulation that has hallmark laboratory and pathologic findings. It’s a clinical diagnosis with variable phenotypes, courses and tempo, with both inflammatory and non-inflammatory features. It has acute and long-term morbidities, immunomodulatory treatment paradigms and racial and sex disparities. Further, lupus and sarcoidosis have a similar prevalence in the U.S. Several diseases, such as vasculitis and inflammatory myositis, are rarer.
“You’d think that if we’re comfortable with [managing] lupus, we’d also be comfortable with [managing] sarcoidosis. We should be taking a stronger role. There are many reasons we haven’t, but we should get over ourselves,” he said.
