“Now that we have this formulation of triamcinolone hexacetonide available, it’s probably going to pick up use again,” explains Dr. Cron, “because the second-best intra-articular steroid may only last two months to keep the arthritis at bay, whereas this one may last a year.”
Intra-articular triamcinolone hexacetonide may be particularly helpful for patients who have only one or two joints with active disease at presentation, or if a patient has one or two joints that haven’t responded to other interventions, he notes.
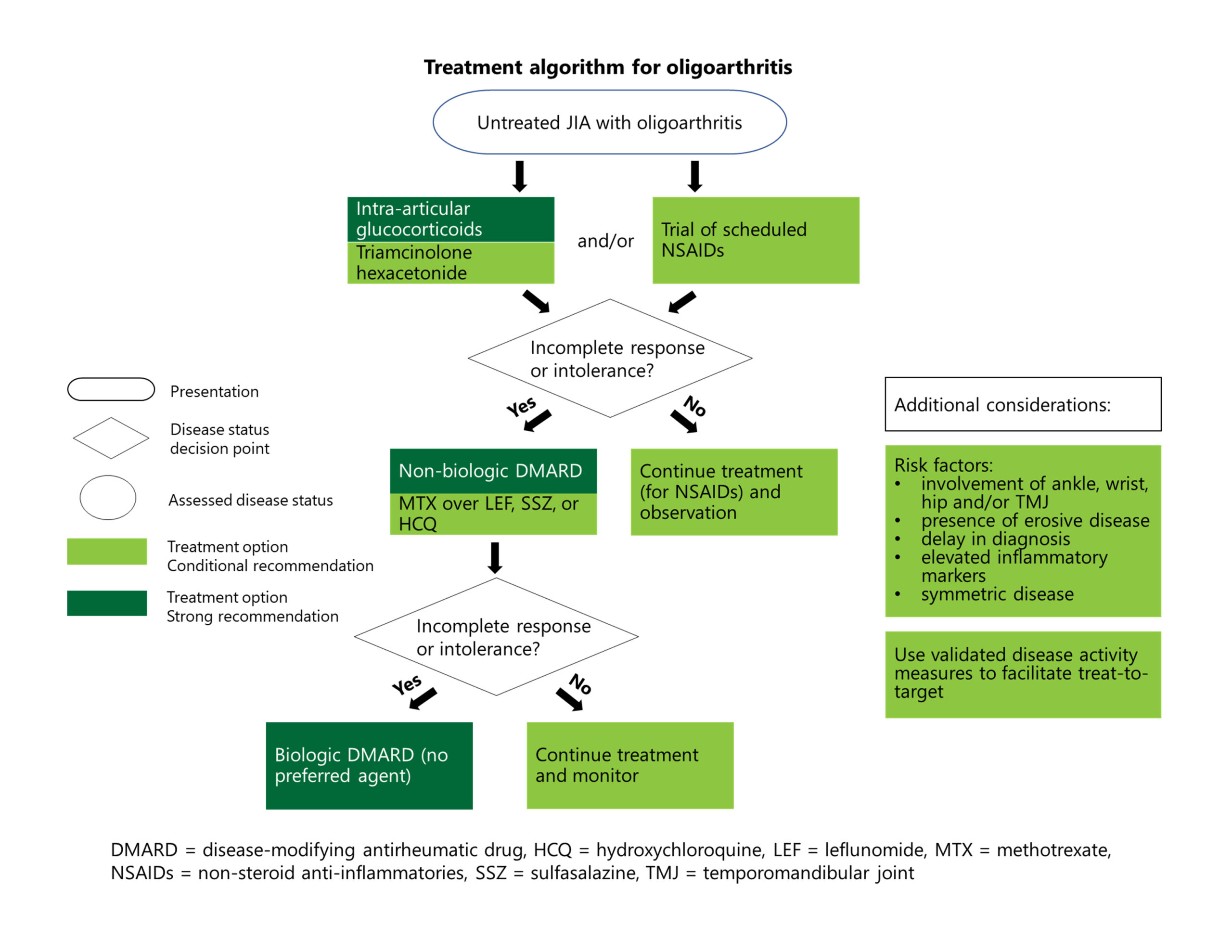
Recommendations: After a brief trial with NSAIDs, if the disease is still inadequately treated or if treatments are not tolerated, conventional synthetic (cs) DMARDs are strongly recommended. If the disease is still not adequately controlled, biologic (b) DMARDs are strongly recommended.1
However, the guideline writers were careful to point out that this rough treatment algorithm should be interpreted in the clinical context and modified, if needed. For example, providers may need to rapidly escalate therapies in the context of poor diagnostic features, such as elevated inflammatory markers, erosive disease, enthesitis or involvement of the ankle, wrist, hip, sacroiliac or temporomandibular joints.
Although methotrexate is recommended over other csDMARDs, the guideline writers expressed no preference in terms of bDMARDs, given the lack of available comparative evidence.
Dr. Onel notes that tumor necrosis factor (TNF) inhibitors are the most commonly used bDMARDs in childhood arthritis, so we have the most clinical experience and data about their safety and effectiveness. However, given the limited number of head-to-head trials of biologics, other bDMARDs, such as abatacept or interleukin (IL) 6 inhibitors, could be used in this context.
Treatment for TMJ Arthritis
Recommendations: For patients with active disease, the panelists conditionally recommend a brief trial of NSAIDs as part of the initial therapy, conditionally recommend against oral glucocorticoids, but conditionally recommend in favor of intra-articular glucocorticoids.1
Recommendations: If symptoms are still not well controlled after treatment with NSAIDs and/or intra-articular glucocorticoids, csDMARDs are strongly recommended. bDMARDs are conditionally recommended at this point or after inadequate response to csDMARDs.1
TMJ arthritis can occur alone or in tandem with arthritis in other joints. Dr. Onel points out that the guideline writers wanted to include specific recommendations on TMJ because of its potentially devastating complications. “You just can’t overstate how important it is that people be able to open their mouths. It definitely needs to be treated aggressively.”