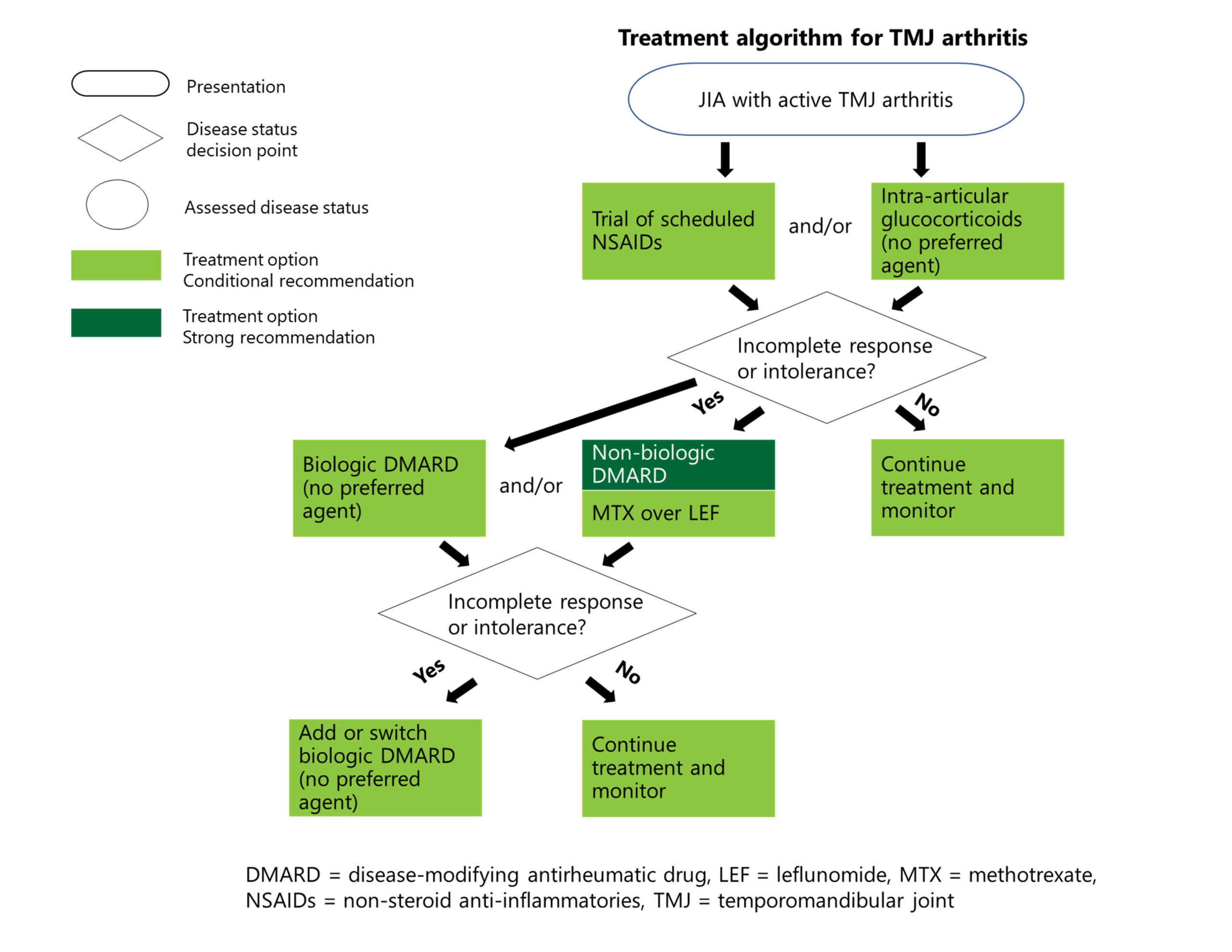
TMJ arthritis has powerful deleterious growth effects on children, on the midface as well as the jaw, Dr. Cron adds. “It is a very commonly involved joint, but one that is very difficult for us to treat; it remains one of our problematic joints,” he says.
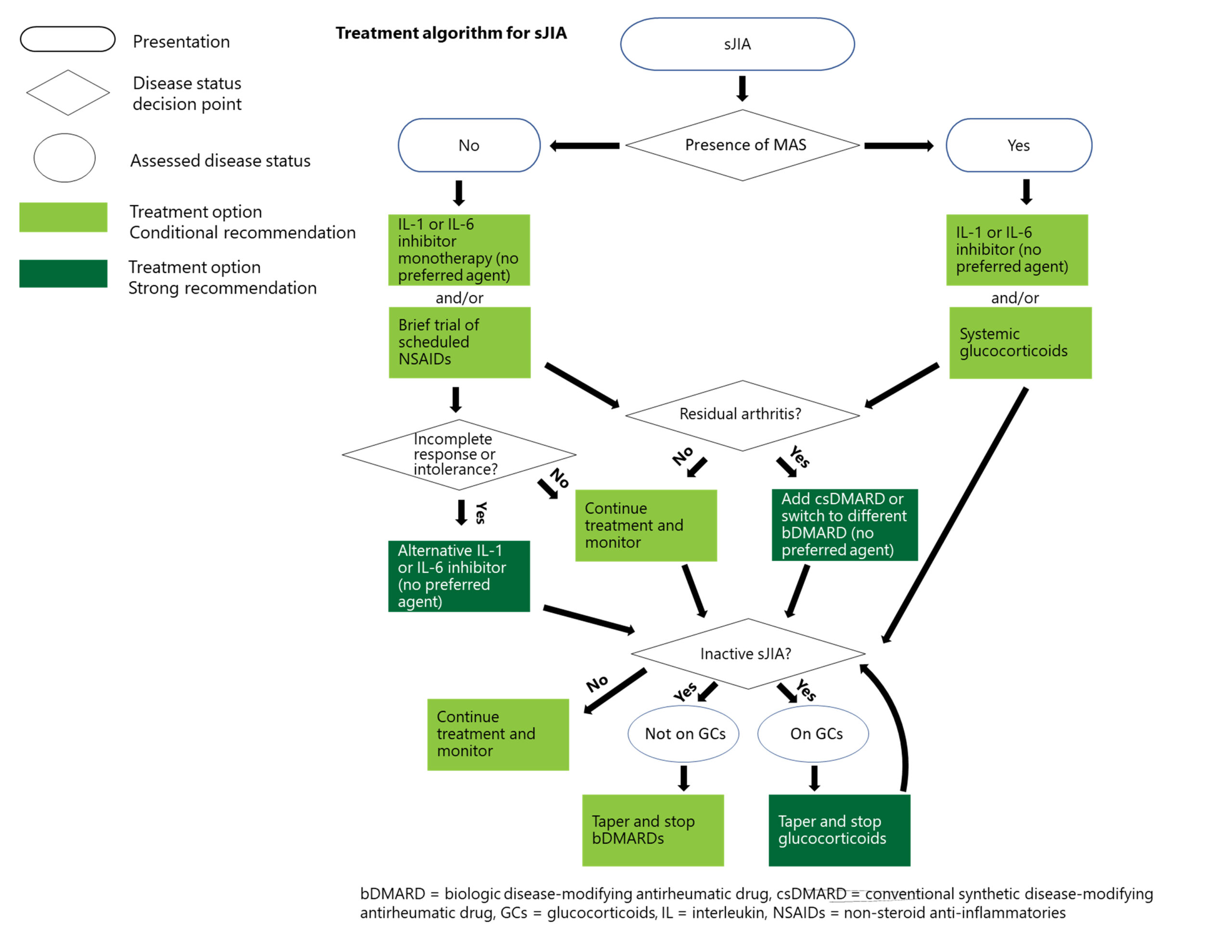
Treatment for Systemic JIA
Recommendations: For patients with systemic JIA without macrophage activation syndrome, IL-1 inhibitors, IL-6 inhibitors or NSAIDs are conditionally recommended as initial treatment, but with rapid escalation if response to NSAIDs is not fast and complete. Both oral glucocorticoids and csDMARDs are conditionally recommended against as initial therapy. IL-1 and IL-6 inhibitors are also strongly recommended over csDMARDs for treatment escalation.1
Recommendations for systemic JIA with macrophage activation syndrome are similar, but glucocorticoids are conditionally recommended as part of initial therapy, with tapering and discontinuation as soon as the disease is inactive.1
“When we say that the first-line treatment for systemic JIA is a biologic—not an NSAID or steroids or a conventional DMARD—that is really an extraordinary statement in terms of how much the field has moved,” Dr. Onel notes. “We have concerns with using biologics early in disease, but that has to be balanced with memories of the long-term outcomes for these children, which were terrible.”
With its internal organ involvement and severe, acute nature, systemic JIA requires more aggressive intervention compared to other forms of JIA—even more so when it is accompanied by macrophage activation syndrome.
“We wanted to make it clear that although we urge avoidance of daily steroids, basically all bets are off when there is also [macrophage activation syndrome],” Dr. Onel explains. “These children are extremely ill and need to be treated aggressively.”
Other Recommendations
Recommendations: All patients should receive baseline laboratory testing before treatment initiation for all medications. The guideline authors also provided guidance with respect to repeat testing for specific medications, such as screening with complete blood count and liver and kidney function tests every three to four months for patients taking methotrexate.2
Dr. Onel points out that this area is a good example of where shared decision making is important because families differ in how they perceive the burden and benefits of repeat blood tests. “You can’t tell how people will feel without asking,” she says. “We are trying to keep children safe without tormenting them by drawing their blood unnecessarily.”