Finger
Most students had not practiced scanning the first metacarpalphalangeal (MCP) joint, and so had difficulty with the volar/palmar views. Some students held the transducer perpendicular to the palm rather than perpendicular to the thumb (they should have aimed the beam directly at the longitudinal aspect of the thumb flexor tendons and the underlying bones rather than along the anatomic sagittal plane). Although we focus on MCP 2–4 in patients with inflammatory arthritis, and many ultrasound protocols skip the first MCP, this joint can certainly be involved, and the scanning technique needs to be slightly adjusted to account for the differences in anatomy, including the consistent presence of the two thumb sesamoid bones.
Most students did focus attention on the synovial recess, which extends proximally to the joint cleft. On the volar side of the MCP, the synovial recess is best visualized proximal to the palmar plate. Earlier in their training, many fellows made the mistake of assessing Doppler in the joint cleft but forgetting to include the proximal synovial reflection in the Doppler box (see Figure 3). By the time of the practical exam, our mentors gave all fellows a thumbs-up on this technique (sic, PD).
When performing a RhUS examination, it’s critical to sweep the transducer across the entire target structure, or asymmetrically located pathologies (e.g., swollen synovium, effusion, erosion) may be missed.
Wrist
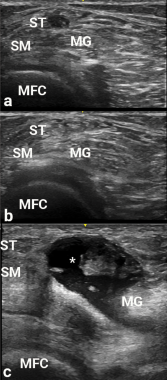
Figure 2
Images a, b and c are transverse
views of the medial popliteal space. Due to anisotropy, the semitendinosus area (adjacent to ST) is hypoechoic in appearance, and could be confused with a popliteal cyst. The ST become hyperechoic in b after transducer angle adjustment, thereby making the potential cyst disappear. In c, a real popliteal cyst (asterisk) is apparent between the semimembranosus (SM) and medial gastrocnemius (MG), and over the medial femoral condyle (MFC).
In obtaining the volar/palmar transverse view of the wrist, many found it challenging to visualize the median nerve without having the flexor tendons appear too dark due to anisotropy. Angling the probe/sound waves toward the elbow helps resolve this issue. This positioning requires a lot of nerve (sic, PD again).
Differentiating the extensor retinaculum from tenosynovium on the dorsum of the wrist presented an additional trial for some. The normal retinaculum should be a focus of attention in scanning healthy wrists for this reason.
The extensor carpi ulnaris (ECU) can be difficult to image without anisotropic artifact due to its serpiginous course. Radially deviating the wrist can help overcome this difficulty by straightening the ECU to minimize anisotropy.


