In this retrospective study, the TriNetX electronic health records database was used to identify 5,142 patients with giant cell arteritis, 16% of whom received treatment with tocilizumab. Incident gastrointestinal perforations among patients with giant cell arteritis treated with tocilizumab occurred at a rate of 2.0 per 1,000 person-years. Among patients with giant cell arteritis not treated with tocilizumab, the incidence rate was 3.4 per 1,000 person-years.
Gastrointestinal perforation was associated with diverticular disease (relative risk 3.51) and intravenous methylprednisolone (relative risk 5.41). However, when the dataset was used to emulate a clinical trial, using a clone-censor-weight approach that attempts to eliminates the influence of glucocorticoids on the outcome of interest, tocilizumab exposure was not associated with an increased risk of gastrointestinal perforation (hazard ratio 1.05).
Patients with giant cell arteritis who are deemed to be at high risk of poor outcomes are more likely to be treated with both high-dose, intravenous glucocorticoids and tocilizumab. Clinically, therefore, it is difficult to tease apart the relationship between each of these interventions and various untoward events, including gastrointestinal perforation. This novel analysis implies that among patients with giant cell arteritis, high-dose glucocorticoids may largely be to blame for the increased risk of gastrointestinal perforation attributed to tocilizumab. Reassuringly, this study confirms that the overall risk of gastrointestinal perforation among patients with giant cell arteritis is low, whether or not they receive tocilizumab therapy.
5. Spondyloarthritis-spectrum disorders and Takayasu arteritis. Kerem Abacar, Sema Kaymaz-Tahra, Özün Bayındır, et al. Abstract O-078.
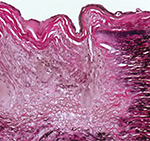
Takayasu arteritis is the archetypal large vessel vasculitis, which is associated with a granulomatous inflammation of the aorta and major arterial branches. Takayasu arteritis can also be associated with extravascular manifestations, including retinopathy and arthritis.
Abacar et al. reviewed 350 patients with Takayasu arteritis followed in 12 clinics in Turkey for evidence of disease manifestations associated with HLA-B27. Of these patients, eight (2.2%) had inflammatory bowel disease, eight (2.2%) had psoriasis and 20 (5.7%) had axial spondyloarthritis. Patients with these diagnoses had similar patterns of vascular involvement when compared with patients who had Takayasu arteritis but lacked these features. However, patients with these additional diagnoses tended to develop evidence of Takayasu arteritis at a younger age (26 vs. 32 years old).
This study indicates that patients with inflammatory bowel disease, psoriasis or axial spondyloarthritis may be at increased risk of developing Takayasu arteritis, and increased clinical surveillance required by the spondylitis-spectrum disorder leads to an earlier diagnosis of vasculitis.