Farber disease usually presents in patients within the first year of life. A review of 31 patients published in the medical literature shows the median time for onset of first symptoms as 4 months old.7-29 Only two patients were reported to have presented as late as 20 months.3,16 Our patient’s presentation with hoarseness of voice at age 18 months certainly represents the upper end of the spectrum of age at first presentation. It’s important to note that our patient also developed arthritis-like symptoms at 30 months of age, which is later than most patients with Farber disease. It is not surprising, then, that he was initially diagnosed with juvenile idiopathic arthritis.
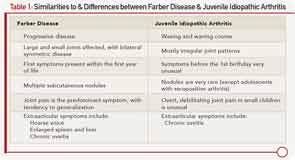
The similarity between JIA and Farber’s disease has been noted previously. Farber disease can be divided into seven types, of which only the first three comprise more than seven patients reported so far.4,30 According to this classification, this patient would belong to Type 3, which is often regarded as a mild form of the disease. Patients still suffer from the classical triad of symptoms, but they experience slight or no neurological disease and may live well into adulthood. Mild cases of Farber disease are especially susceptible to misdiagnosis due to the under-representation of mild Farber disease cases in the medical literature. However, the nodules and accompanying hoarseness, as well as the early onset and unrelenting progress of the disease provide important clinical clues. A phenotypic comparison of juvenile idiopathic arthritis and Farber disease is shown in Table 1.
With enzyme replacement therapy in preclinical development, current treatment options in Farber disease are limited. The patient has benefited from intensive physical therapy, but still shows unrelenting, progressive disease with increasing contractures and functional impairment. It’s interesting to observe that anti-tumor necrosis factor medication can be effective in alleviating joint pain in this disease, despite its inability to halt its progression.
The only curative treatment for Farber disease available at this time is stem cell transplantation. In cases without neurological involvement, this treatment leads to considerable improvement.31 However, stem cell transplantation depends on the availability of suitable donors and still carries significant risks. Studies performed on mice with acid ceramidase deficiency have shown the effectiveness of enzyme replacement therapy. Treatment of these mice with a single injection of human acid ceramidase-encoding lentivector resulted in enhanced growth, decreased ceramide levels and cellular infiltrations, and increased lifespan. The severity of the disease was greatly diminished.32 In theory, Farber disease could be amenable to treatment with enzyme substitution, similar to other sphingolipidoses.33