A post-hoc analysis showed upadacitinib is safe and effective for treating RA patients when used with methotrexate or non-methotrexate csDMARDs…


A post-hoc analysis showed upadacitinib is safe and effective for treating RA patients when used with methotrexate or non-methotrexate csDMARDs…

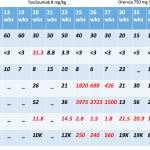
In a 24-month clinical trial, tofacitinib proved safe and effective in combination with methotrexate in adult patients with RA…
Will Boggs MD |
NEW YORK (Reuters Health)—Monotherapy with the JAK1-selective inhibitor upadacitinib is effective in patients with active rheumatoid arthritis who have an inadequate response to methotrexate, according to results from the SELECT-MONOTHERAPY phase 3 trial. As many as two-thirds of patients with rheumatoid arthritis receiving methotrexate monotherapy fail to achieve satisfactory disease control. Oral therapy with upadacitinib…
SNOWMASS VILLAGE, COLO.—Even in the era of treat to target, cardiovascular disease risk remains elevated and is a major source of mortality and morbidity in patients with rheumatoid arthritis (RA). Screening and management of cardiovascular risk in these patients is critical to ensure these patients are identified and treated. At the 2019 ACR Winter Rheumatology…

CHICAGO—Once methotrexate enters a cell through the reduced folate carrier (RFC), which thinks it is picking up folate, the drug is polyglutamated. It is this polyglutamate methotrexate that provides the actual clinical effect. These methotrexate polyglutamate “species” are added and lost over time, but it’s a slow process. What difference does it make whether a…
Note: Although originally posted in January 2018, the advice below remains valid. We see this issue recur each year. As we begin another new year, many rheumatology practices will again receive prior authorization requests from Medicare Part D for all methotrexate prescriptions. When methotrexate is used as a chemotherapeutic drug, it’s covered by Part B,…

Recent post-hoc analyses of two Phase 3 clinical trials show that RA patients with high interleukin 6 levels taking sarilumab experienced improved symptoms and less joint damage than those using other treatments…
Mohammad A. Ursani, MD, RhMSUS, & Jaecel Shah, MD |
Primary Sjögren’s syndrome is a systemic autoimmune condition noted for findings of xerostomia, keratoconjunctivitis sicca and focal lymphocyte infiltrate in salivary glands.1 In the initial publications regarding keratoconjunctivitis sicca, Henrik Sjögren, a Swedish ophthalmologist, described a group of 19 women with dry eyes, some of whom had other organ dryness and inflammatory infiltrates.2,3 The syndrome…

In a study, RA patients taking upadactinib monotherapy experienced less pain and morning joint stiffness than methotrexate-treated patients…
Erin Hammett, DO, & Edward Skol, MD |
Polymyalgia rheumatica (PMR) is an inflammatory rheumatic condition characterized by pain and morning stiffness at the neck, shoulders and hip girdle. It can be associated with giant cell arteritis (GCA); in fact, the two disorders may represent a continuum of the same disease process. This case describes a patient who initially refused treatment for PMR…