 Previous studies have shown that interleukin 1β (IL-1β) inhibitors can shorten gout flares. But prevent the attacks in the first place?
Previous studies have shown that interleukin 1β (IL-1β) inhibitors can shorten gout flares. But prevent the attacks in the first place?
Canakinumab targets IL-1β and was recently investigated in the Canakinumab Antiinflammatory Thrombosis Outcome Study (CANTOS). The randomized, double-blind, placebo-controlled trial was not designed to study gout, but rather to examine canakinumab’s effect on a cardiovascular endpoint. Patients in the trial were randomized to receive placebo or one of three different canakinumab dosages once every three months. The study demonstrated that canakinumab reduces major adverse cardiovascular events.1
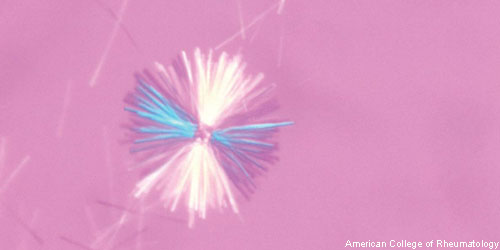
An exploratory analysis of the CANTOS trial data reveals that patients who received quarterly canakinumab experienced significantly reduced risk for gout flares even though they did not experience changes in serum uric acid levels. Daniel H. Solomon, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues suggest these data may be relevant as researchers develop gout therapies targeting the IL-1β pathway of innate immunity. The results of their analysis of gout data from the CANTOS trial were published online in the Annals of Internal Medicine.2
The patients in the CANTOS trial had a median baseline serum uric acid (SUA) concentration of 362.9 µmol/L (interquartile range: 309.3–428.3 µmol/L). The investigators followed patients for a median of 3.7 years and tracked the incidence rate of gout flares in patients grouped by their SUA concentration. They note in the study that the concentrations of SUA can change over time and the solubility of uric acid in blood is extremely variable from person to person.
The researchers found that patients with an SUA level of 404.5 µmol/L or less had an incidence rate of gout of 0.28 per 100 person-years. Patients with an SUA between 404.6 and 535.3 µmol/L had a rate of 1.36, while patients at 535.4 μmol /L or higher had a rate of 5.94. Although canakinumab did not affect SUA levels, it significantly reduced rates of gout flares at all baseline SUA concentrations relative to placebo. The hazard ratios for the three groups were 0.40, 0.48 and 0.45. Thus, the CANTOS trial revealed large risk reductions for incident gout—approximately 50%—at all three canakinumab doses, across all levels of baseline SUA, including baseline SUA levels that are considered normal.
The authors emphasized that the risk reductions for gout flares did not depend on the dose of canakinumab.
“Whereas others have shown the potential benefits of IL-1β blockade during acute gout attacks, we believe our data to be the first randomized controlled demonstration of gout prevention through IL-1β blockade,” write the authors in their discussion. “Although perhaps not surprising, this observation has considerable clinical relevance. Because the benefits were profound and were seen with the lowest canakinumab dosage (50 mg every 3 months), our data provide proof of concept that low-dose IL-1β inhibition might prevent the incidence of gout attacks, particularly among patients in whom current therapies have failed.”
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
References
- Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017 Sep 21;377(12):1119–1131.
- Solomon DH, Glynn RJ, MacFadyen JG, et al. Relationship of interleukin-1β blockade with incident gout and serum uric acid levels: Exploratory analysis of a randomized controlled trial. Ann Intern Med. 2018 Oct 16;169(8):535–542.