Assessing Dactylitis
Dactylitis diagnosis is clinical. An examination sees fusiform swelling of fingers or toes with associated variable erythema and locally increased temperature, and tenderness in the acute phase. Differential diagnosis includes infection, crystalline disease and sarcoidosis.
The only PsA-specific dactylitis index is the Leeds enthesitis index, performed with a small measurement tool (the Leeds dactylometer) and scored as a weighted sum of dactylitic digits upon assessment of all 20 digits.13 A digit is defined as dactylitic if its circumference measures 10% higher than the contralateral digit/or reference norms.
For scoring, the weights applied are 0–1 (i.e., 0 is not tender, 1 is tender) for the basic Leeds index, and 0–3 (i.e., 0 has no tenderness and 1–3 indicates increasingly higher degrees of tenderness) for the initial index. The Leeds index counts only acute dactylitis.
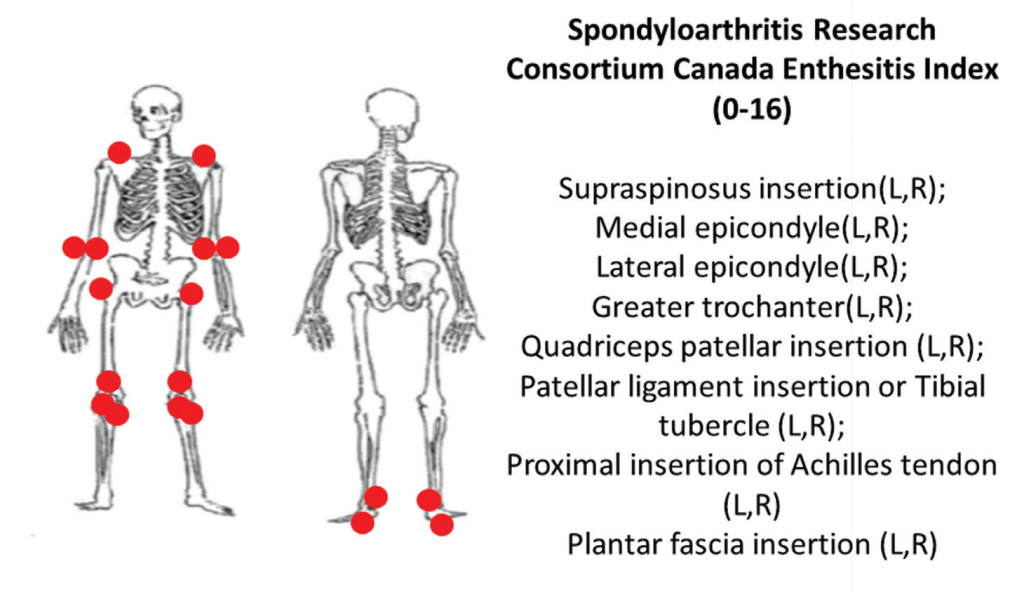
6A: The Spondyloarthritis Research Consortium of Canada clinical enthesitis index.
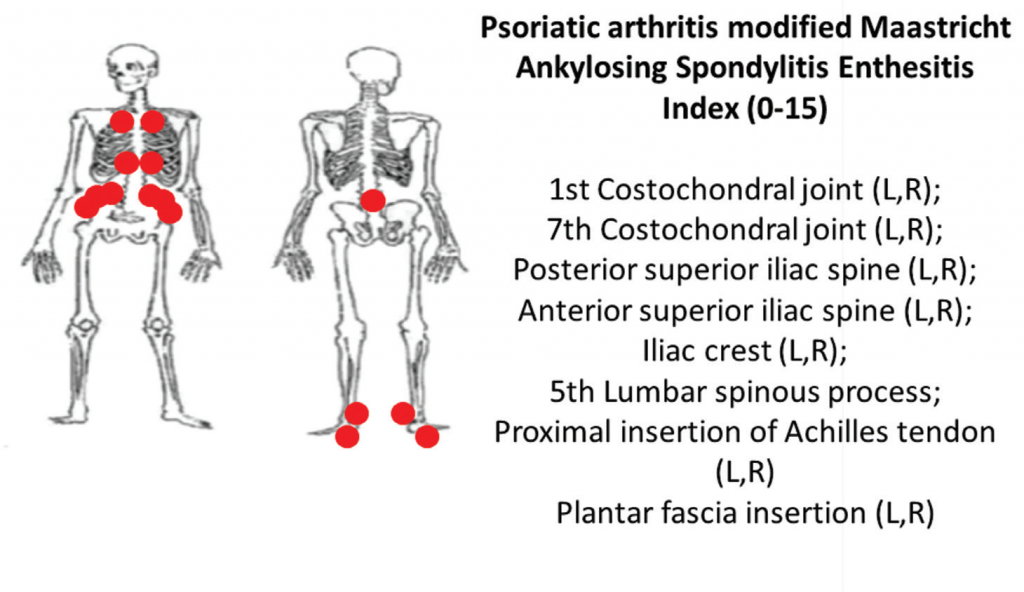
6B: The PsA-modified Maastricht Ankylosing Spondylitis clinical enthesitis index (PsA MASES).z
Dactylitis can also be demonstrated on ultrasound and MRI, as described above.
Assessing Enthesitis
Multiple clinical and ultrasound enthesitis indices exist or are in development. Although clinical enthesitis indices are the most feasible to perform, they are also the most difficult to align with the true pathophysiological process underlying enthesitis because they rely on the assumption that tenderness to pressure is representative of PsA entheseal inflammation. Confounding factors for PsA enthesitis on clinical or imaging assessment include pain attributable to anatomical structures in proximity to entheses, degenerative processes, physiological enthesial complex aging and overuse/injury, among others.
Two comprehensive clinical enthesitis indices include the Spondyloarthritis Research Consortium of Canada enthesitis index (SPARCC) and the PsA modified Maastricht Ankylosing Spondylitis Enthesitis Score (MASES). Both have been used in PsA clinical trials. SPARCC assesses entheses that are predominantly peripheral by tenderness to standardized pressure applied on examination of 18 sites. The SPARCC score range is 0–16, and higher scores indicate more entheseal sites are tender.
Using the same examination technique, the PsA-modified MASES index assesses axial and lower extremity entheses at 15 sites with a score range of 0–15. Higher PsA modified MASES scores indicate more entheseal sites involved (see Figures 6A and 6B).
Imaging studies, particularly ultrasound, are more sensitive at detecting peripheral enthesitis than clinical exams, and they can identify subclinical entheseal involvement as well as characterize anatomical changes more specific to an inflammatory disease. Both inflammatory changes (e.g., tendon thickening and hypoechogenicity near insertion, bursitis, Doppler enhancement, etc.), as well as damage changes (e.g., bone erosions, enthesophytes, etc.) can be seen (see Figure 7).12


