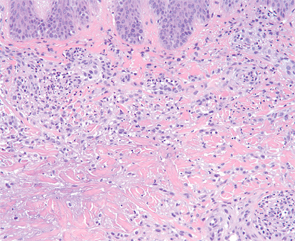
Figure 4: Higher magnification demonstrates aggregates of neutrophils and an interstitial arrangement of histiocytes. (Hematoxylin-eosin stain; original magnification: x400.) Photomicrograph courtesy of Timothy McCalmont, MD.
In patients without a preceding diagnosis of a connective tissue disorder or rheumatoid arthritis, a comprehensive evaluation is warranted and should include serologic testing for antinuclear antibodies, antineutrophil cytoplasmic antibodies (ANCAs), rheumatoid factor (RF) and cyclic citrullinated peptide, as well as a complete blood count with differential and a chest X-ray. In select cases, serum protein electrophoresis and/or immunofixation electrophoresis, viral hepatitis and HIV testing should be considered.2 Even in patients with an established systemic disease, a careful search for an underlying cause is warranted because the development of PNGD may herald the onset of an additional inflammatory or infectious process.
Because PNGD is a rare disorder, evidence for its treatment is anecdotal and limited to case reports and small series. In up to 20% of cases, PNGD resolves without intervention. Therefore, observation alone may be an acceptable management approach.2 In persistent cases, therapy should be directed toward the underlying systemic cause, as optimization of the systemic disorder often improves the skin disease. PNGD-specific treatment may be needed when a systemic association cannot be identified or when the associated condition is under control yet the skin disease persists. In such cases, dapsone, colchicine, and intralesional and systemic corticosteroids are reportedly effective.2,6
Although a benign and often self-limited condition, PNGD is an important diagnosis to recognize, because it serves as a skin sign of internal disease, particularly of autoimmune origin. Appropriate management mandates a thorough investigation to identify a precipitating cause.
Incorrect Answers
A. Rheumatoid nodules: Rheumatoid nodules are firm, semi-mobile nodules that are present in up to 20% of patients with rheumatoid arthritis, most commonly in the setting of high titers of rheumatoid factor. Similar to PNGD, these lesions often cluster around joints and on extensor surfaces including the elbows and hands (i.e., trauma-prone sites). Unlike PNGD, rheumatoid nodules can enlarge to several centimeters in size and may involve visceral organs. Accelerated rheumatoid nodulosis following initiation of methotrexate or anti-TNF-α therapy has been reported. By histopathology, rheumatoid nodules are composed of eosinophilic fibrin surrounded by a palisade of histiocytes characteristically located in the deep dermis and subcutis; unlike PNGD, neutrophils are absent. The lack of crusting, umbilication, and ulceration on clinical examination as well as the size and the distinct histopathologic features are useful to distinguish rheumatoid nodules from PNGD.