
Figure 3. The patient had flexion contractures of her knees.
months from symptom onset was also found to be associated with improved prognosis. A role for immunosuppressive agents in conjunction with corticosteroids has also been discussed in the literature as possibly improving treatment outcomes.2,6 Methotrexate is often the most commonly used corticosteroid-sparing agent; however, the efficacy of mycophenolate mofetil, azathioprine, tumor necrosis factor inhibitors and other therapies has been detailed in small case series. In one retrospective study of 34 patients, methotrexate used in combination with corticosteroids was needed in 44% of patients due to an unsatisfactory response to corticosteroids alone.6
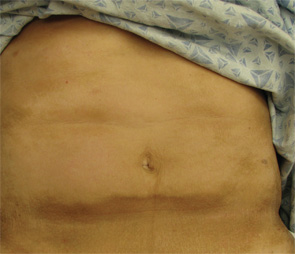
Figure 4. The exam also revealed indurated plaques on the patient’s abdomen.
Because there can be an association with underlying malignancy, most commonly hematologic and myelodysplastic disorders, we advise serum protein electrophoresis and immunofixation testing in all patients. Those patients with cutaneous findings overlying the joints, or those with contractures upon presentation, should receive aggressive physical and/or occupational therapy to prevent morbidity.
Incorrect Answers
A. Systemic sclerosis: Systemic sclerosis and EF can most often be differentiated based solely on clinical exam. The cutaneous findings of systemic sclerosis include sclerosis and skin thickening involving the distal digits; proximal nail fold changes, including erythema and dilated capillaries; and sclerodactyly. Patients classically have Raynaud’s disease. As discussed above, our patient has normal skin laxity overlying the fingers, no proximal nailfold changes and no history of Raynaud’s to suggest systemic sclerosis. In addition, EF patients almost uniformly lack visceral involvement.
B. Hypereosinophilic syndrome: Hypereosinophilic syndrome is characterized by marked peripheral eosinophilia counts (>1,500/microliter) for a period of at least six months without evidence of an alternative etiology. Patients also have symptoms of multiorgan involvement. Fifty percent of patients have cutaneous findings that include urticaria, angioedema and mucosal ulcers, as well as erythematous macules, papules and nodules on the trunk and extremities. Although both entities can have a peripheral eosinophilia, hypereosinophilic patients do not exhibit the cutaneous findings of EF.
C. Lipodermatosclerosis: Lipodermatosclerosis most commonly develops in the setting of long-standing venous insufficiency. Acute symptoms include erythema, tenderness and warmth of the medial ankles. Cutaneous findings later evolve into sclerotic hyperpigmented plaques that resemble an “inverted champagne bottle” on the lower legs. Lipodermatosclerosis may be unilateral or bilateral. The localization of lipodermatosclerosis on the medial lower extremities in the setting of chronic venous insufficiency differentiates this condition from EF. In addition, histopathological examination reveals a lobular panniculitis instead of a deep fasciitis, and laboratory abnormalities are uncommon in lipodermatosclerosis.


