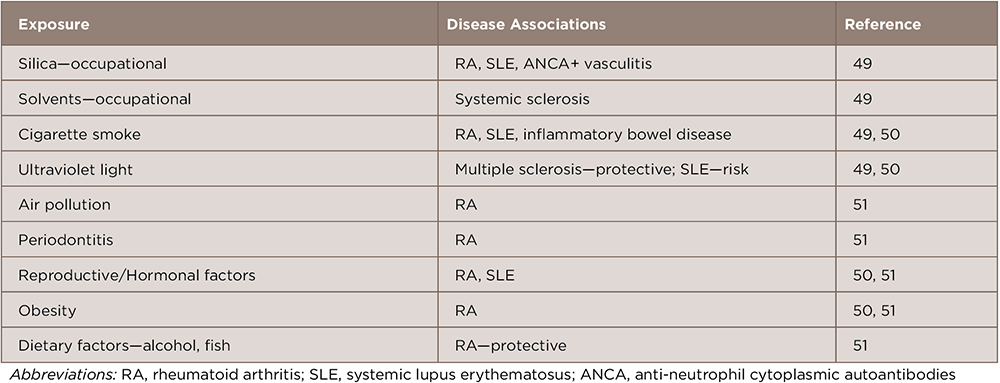
Systemic autoimmune diseases are thought to result from immune dysregulation in genetically susceptible individuals who were exposed to environmental risk factors. Many studies have identified genetic risk factors for these diseases, but concordance rates among monozygotic twins are 25–40%, suggesting that nonheritable environmental factors play a more prominent role.1,2 Through carefully conducted epidemiologic and other approaches, environmental factors for adult forms of these diseases have been identified (see Table 1).
Here we review emerging data for pediatric systemic autoimmune diseases, particularly juvenile idiopathic arthritis (JIA). Although most studies have been conducted in JIA, we also include data for pediatric systemic lupus erythematosus (SLE), juvenile dermatomyositis (JDM) and Kawasaki disease, a systemic vasculitis in young children. Our focus is primarily on case-control studies, including those that compare subgroups to identify severity factors.
Seasonality & Temporal & Spatial Clustering
Variations in the onset of disease suggest that seasonal environmental factors may be involved in the etiology. Seasonal variations in birth distribution suggest that seasonal neonatal or perinatal exposures may have a role in the development of disease. Several studies of systemic autoimmune diseases in children found seasonal variation in disease onset or in birth distributions.
Although a study of systemic JIA found no seasonality in disease onset in Canada during a 12-year period, there was a seasonal pattern in onset in the Prairie region, with peaks in the fall and early spring, but these peaks did not correlate with viral or Mycoplasma pneumoniae seasonal outbreaks in that region.3 A large study of JIA in Israel showed seasonality in birth dates, with a peak from November to March and nadir in the summer months compared with the general population, but a Danish national study of JIA found no birth seasonality and no temporal or spatial clustering of cases.4,5
In juvenile myositis, there was no overall seasonality to birth dates in a national study population, but subgroups of patients had seasonal birth distributions, including Hispanic patients, who had a peak birth seasonality in mid-October, and anti-p155/140 autoantibody negative JDM patients, who had a peak birth seasonality in July.6
(click for larger image)
Table 1: Possible Environmental Risk Factors for Systemic Autoimmune Diseases in Adults
A global analysis of Kawasaki disease using data from 25 countries over three decades demonstrated peak disease onset in the winter months, January through March, in the northern hemispheres, with a nadir in August and September.7 Active surveillance of Kawasaki disease cases in a five-year period in San Diego County, Calif., demonstrated significant clustering of cases within a space–time interval of 3 kilometers and three to five days, suggesting a potential infectious or other environmental trigger operating within a relatively small geospatial window.8


