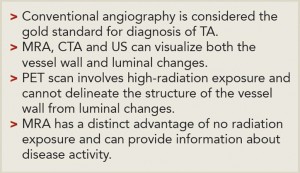
The rupture of aneurysms in Takayasu’s arteritis can be catastrophic and, unlike atherosclerotic aneurysms, size may not be the only consideration for surgery.
Image Credit: BioMedical/shutterstock.com
A healthy 30-year-old Indian male was performing his routine workout in the gym when he developed giddiness and transient blackouts. He thought it was due to exercising excessively. Over the next month, he developed a low-grade fever and started feeling lethargic, to the extent that he was unable to exercise or work.
He was admitted to the hospital with the above complaints and was found to be hypertensive. Investigatory reports showed elevated inflammatory markers with an erythrocyte sedimentation rate (ESR) of 100 mm/hour and C-reactive protein (CRP) of 96 mg/dL. An ultrasound study of the abdomen showed a shrunken left kidney and altered Doppler signals emanating from the proximal left renal artery suggestive of renal artery stenosis.
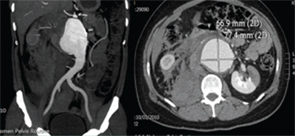
Figure 1. CT-angiography showing ruptured abdominal aortic aneurysm with a retroperitoneal and intraperitoneal hematoma with left renal infarct.
CT-aortography demonstrated an abdominal aortic aneurysm extending from the origin of the superior mesenteric artery (SMA) to the aortic bifurcation and measuring 11.9 cm in length and 4 cm in width. The origins of both renal arteries were involved in the aneurysm. There was focal ectasia of both carotid bulbs and dilation and stenosis of both subclavian arteries at their origins. Mild aneurismal dilation of the left distal external iliac and left femoral artery was seen. A PET-CT showed active inflammation involving the aortic arch, origin of the left common carotid, ascending aorta, both carotid and femoral arteries. He was diagnosed with Takayasu’s arteritis (TA), and he was treated with prednisolone 60 mg/day and methotrexate 15 mg/week. Over the course of one year, he had a good response to treatment, and the steroids were tapered slowly to 5 mg/day. He discontinued therapy and did not keep future appointments.
A year later, he presented to the emergency department with acute abdominal pain and hypotension. Imaging confirmed a ruptured aortic aneurysm with a retroperitoneal and intraperitoneal hematoma. There was extensive infarction of the left kidney (see Figure 1, left). His echocardiogram showed dilation of the aortic root (3.6 cm) with an aneurysm of the sinus of Valsalva. He underwent emergency surgical repair of the aortic aneurysm using a Dacron graft. Post-surgery, he had temporary renal shutdown, which necessitated short-term hemodialysis. He recovered well and was maintained on prednisolone and methotrexate for another four years. Serial ESR and CRP levels conducted between 2010 and 2014 were in the normal range.