Upon arrival, he denied any prior episodes of pulmonary or joint symptoms. He did report noticing some dryness of his hands with minimal scaling at the onset of these symptoms. He did not have any other rashes, eye problems, chronic sinus issues, oral/nasal/genital sores, Raynaud’s phenomenon, photosensitivity, sicca symptoms, dysphagia, aspiration, abdominal pain, neuropathic symptoms, or bladder symptoms.
On examination he was afebrile with a temperature of 98.9º F, a pulse of 85/min, blood pressure of 124/83 mmHg, respiratory rate of 18.
There was no sinus tenderness. Fine inspiratory crackles at both bases were heard on pulmonary examination. Cardiac exam was unremarkable. He had a faint scaly rash on the palmar aspect of some of his fingers. There were no nail-fold capillary changes. He had noticeable tenderness and swelling in the metacarpophalangeal, proximal interphalangeal, and metatarsophalangeal joints. His back, sacroiliac, and entheseal exams were normal. His neurological examination was normal. No muscle weakness or tenderness was present.
The hemoglobin was 10.5 (13.5–17.5 g/dL), with normal white blood cell and platelet count. Routine serum chemistries and liver function tests were normal. His Westergren erythrocyte sedimentation rate was 46 (0–15 mm/hr) and his C-reactive protein was 21 (0–10 mg/L). Urinalysis, creatinine kinase, hepatitis panel, HIV screen, and serum ferritin were unremarkable.
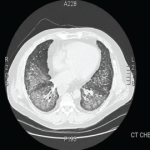
A new chest radiograph showed consolidation in the left lung base, nodular opacities in both lungs, and small bilateral pleural effusions (see Figure 1). A computed tomography (CT) scan of the chest showed multifocal areas of ground-glass and reticular opacities, predominantly in the bilateral lower lobes, along with bronchiectasis (see Figure 2). No cavitary or nodular lesions were identified. Pulmonary function testing (PFT) revealed a restrictive pattern with a forced vital capacity at 53% of expected value and carbon monoxide diffusion capacity at 50% of predicted value. A six-minute walk test resulted in oxygen desaturation to 80% on room air. A transthoracic echocardiogram was normal.
Results of rheumatological workup included a rheumatoid factor (RF) of 119 (0–14 IU/mL), homogenous antinuclear antibody (ANA) pattern with a titer of >1:640, SSA and SSB of 8 (0–0.9 AI), SSB and ribonucleoprotein antibody of 1.4 (0–0.9 AI). Antineutrophil cytoplasmic (ANCA) antibody, Smith, DNA, antiglomerular basement membrane, scl-70, and cyclic citrullinated antibodies were all negative. Serum angiotensin converting enzyme, complement, and cryoglobulins levels were normal.
A CT scan of the sinuses showed soft-tissue opacification of the right maxillary sinus without bony destruction along with multiple subcentimetric lymph nodes.